Dolphin
Senior Member (Voting Rights)
Chiara Gattoni, Asghar Abbasi, Carrie Ferguson, Charles W. Lanks, Thomas W. Decato, Harry B. Rossiter, Richard Casaburi, William W. Stringer,
Two-Day Cardiopulmonary Exercise Testing in Long COVID Post-Exertional Malaise Diagnosis,
Respiratory Physiology & Neurobiology,
2024,
104362,
ISSN 1569-9048,
https://www.sciencedirect.com/science/article/pii/S1569904824001551?via=ihub
Respiratory Physiology & Neurobiology
Available online 28 October 2024, 104362
Two-Day Cardiopulmonary Exercise Testing in Long COVID Post-Exertional Malaise Diagnosis
https://doi.org/10.1016/j.resp.2024.104362
open access
Highlights
BACKGROUND
Long COVID patients present with a myriad of symptoms that can include fatigue, exercise intolerance and post exertional malaise (PEM). Long COVID has been compared to other post viral syndromes, including myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), where a reduction in day 2 cardiopulmonary exercise test (CPET) performance of a two-day CPET protocol is suggested to be a result of PEM. We investigated cardiopulmonary and perceptual responses to a two-day CPET protocol in Long COVID patients.
METHODS
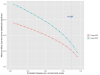
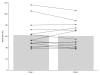
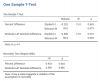
15 Long COVID patients [n=7 females; mean (SD) age: 53(11) yr; BMI = 32.2(8.5) kg/m2] performed a pulmonary function test and two ramp-incremental CPETs separated by 24 hr. CPET variables included gas exchange threshold (GET), V̇O2peak and WRpeak. Ratings of perceived dyspnoea and leg effort were recorded at peak exercise using the modified 0-10 Borg Scale. PEM (past six months) was assessed using the modified DePaul Symptom Questionnaire (mDSQ). One-sample t-tests were used to test significance of mean difference between days (p<0.05).
RESULTS
mDSQ revealed PEM in 80% of patients. Lung function was normal. Responses to day 1 CPET were consistent with the presence of aerobic deconditioning in 40% of patients (V̇O2peak <80% predicted, in the absence of evidence of cardiovascular and pulmonary limitations). There were no differences between day-1 and day-2 CPET responses (all p>0.05).
CONCLUSION
Post exertional malaise symptoms in Long COVID patients, in the absence of differences in two-day CPET responses separated by 24 hours, suggests that post-exertional malaise is not due to impaired recovery of exercise capacity between days.
Key words
cardiopulmonary exercise testing
PEM
exercise tolerance
long COVID
fatigue
deconditioning
Two-Day Cardiopulmonary Exercise Testing in Long COVID Post-Exertional Malaise Diagnosis,
Respiratory Physiology & Neurobiology,
2024,
104362,
ISSN 1569-9048,
https://www.sciencedirect.com/science/article/pii/S1569904824001551?via=ihub
Respiratory Physiology & Neurobiology
Available online 28 October 2024, 104362
Two-Day Cardiopulmonary Exercise Testing in Long COVID Post-Exertional Malaise Diagnosis
https://doi.org/10.1016/j.resp.2024.104362
open access
Highlights
- •
No physiologic differences between day one and two CPET in Long COVID. - •
Questionnaire identification of PEM did not associate with 2-day CPET. - •
PEM was not identified despite repeated exercise testing.
BACKGROUND
Long COVID patients present with a myriad of symptoms that can include fatigue, exercise intolerance and post exertional malaise (PEM). Long COVID has been compared to other post viral syndromes, including myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), where a reduction in day 2 cardiopulmonary exercise test (CPET) performance of a two-day CPET protocol is suggested to be a result of PEM. We investigated cardiopulmonary and perceptual responses to a two-day CPET protocol in Long COVID patients.
METHODS
15 Long COVID patients [n=7 females; mean (SD) age: 53(11) yr; BMI = 32.2(8.5) kg/m2] performed a pulmonary function test and two ramp-incremental CPETs separated by 24 hr. CPET variables included gas exchange threshold (GET), V̇O2peak and WRpeak. Ratings of perceived dyspnoea and leg effort were recorded at peak exercise using the modified 0-10 Borg Scale. PEM (past six months) was assessed using the modified DePaul Symptom Questionnaire (mDSQ). One-sample t-tests were used to test significance of mean difference between days (p<0.05).
RESULTS
mDSQ revealed PEM in 80% of patients. Lung function was normal. Responses to day 1 CPET were consistent with the presence of aerobic deconditioning in 40% of patients (V̇O2peak <80% predicted, in the absence of evidence of cardiovascular and pulmonary limitations). There were no differences between day-1 and day-2 CPET responses (all p>0.05).
CONCLUSION
Post exertional malaise symptoms in Long COVID patients, in the absence of differences in two-day CPET responses separated by 24 hours, suggests that post-exertional malaise is not due to impaired recovery of exercise capacity between days.
Key words
cardiopulmonary exercise testing
PEM
exercise tolerance
long COVID
fatigue
deconditioning