youtube video of Times Radio interview with Karen Gordons father
The woman being denied the NHS care she needs to treat her ME
The woman being denied the NHS care she needs to treat her ME - YouTube
Let me transcribe.
Michael Gordon: They're making her life impossibly difficult in hospital, but they won't give her community care either. The community virtual ward service is saying they won't give IV fluid support on the community. So we can't be in hospital, we can't be at home. So we're just feeling totally helpless and isolated.
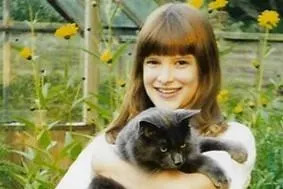
Host: ...treatment for severe ME is complex and difficult. In May, a report by Action for ME concluded that people with the condition are routinely being failed by the health service. Now, when we covered this story, we had a huge response from listeners. We heard from the family of Karen Gordon who is now 36 and has been suffering from ME since she was
10. She can't eat on her own and has to be fed through a tube. Her family says the local NHS trust is not providing the care she needs. And since we spoke at the end of May, things have gotten much worse. Karen's father Michael joins us now. Morning to you, Michael.
Gordon: Hello there.
Host: Tell us in what way things have got much worse.
Gordon: Well, as you said, Karen is fed and water and is administered through a feeding tube, which is called a PEG-J, which goes into the tummy and direct into the bowel. As you've just said, Karen's only recently been discharged from a horrendous 14-month admission with the same hospital group. But over the weekend, the tube blocked, which means that we couldn't actually administer any water or any feed into Karen, and that's her only way of getting feed and fluid. On Monday, we were admitted to the Conquest Hospital at Hastings via the ME service at the Eastbourne DGH as an emergency. But when we got to Hastings, they were told that Karen couldn't have a single room, and neither could Heather stay overnight with Karen.
Host: And why was that, was it because they just didn't have the space?
Gordon: Well, they're saying they didn't have the space into the single room and they're saying it's policy in terms of parents not being able to say with relatives overnight. We did manage to get a stay of execution in that Heather, my wife and Karen's mum, was able to stay last night overnight. But that was after a whole day of extremely long discussions, which was all very stressful. And as you can imagine, it's very stressful for Karen already. The last we want is for this extra aggravation. Karen was quite clear and told the nursing hierarchy that she was unable to cope with a hospital stay without Heather there 24/7. She needs the care that only Heather can provide with the experience that Heather has gained over the many years that we've been supporting Karen. She's got special care needs, which can be immediate, so there's not always nursing staff around. And it can only be done by Heather as she knows how best to help Karen, and that's all we want.
Host: Now, how did the NICE guidelines come into this? Becuase I think the hospitals quote those guidelines saying they have to be followed.
Gordon: Well, yesterday...it's the nursing hierarchy who are absolutely refusing to acknowledge Karen's need, that it's a preference and not a need. Well that's absolutely wrong. It is a need. And
they are saying that the NICE guidelines (the person we spoke to yesterday) are, what they say, guidelines, and if they can't follow them, they can't follow them, or if they don't want to.
Host: So it sounds like, (I mean, again, I don't know, just from what you said) it sounds like, obviously you're going through a very stressful time and you have done since Karen was 10, that's 26 years now. Which must be incredibly wearing on you as a family. And you want the best for her, you don't want her to be on her own. And the hospital presumably are just too stretched to offer you what you want. So what's the way forward, you think?
Gordon: Well, I accept the hospital is stretched. But at the end of the day, as I said, it's not a preference. Karen needs Heather there to provide physical and emotional support. Now it's not ideal for Heather either, we have to think of that, that she's just sort of sitting there on a chair by the side of her room, but she's prepared to do that 24/7 if it helps Karen.
Host: So does that mean, then, that you think implicit in this that the hospital and the hierarchies (you call it) don't consider ME a serious enough condition for that to be the case? For someone to be able to stay with her.
Gordon: Certainly, that's the impression that we're getting from the nursing hierarchy. We've had 23 other hospital admission with Karen and they're always managed to provide a hospital room. Not necessarily immediately, but at least acknowledge that they should be finding a hospital room. And they've always allowed Heather to stay with her, acknowledge the sort of needs that Karen has.
Host: So what's the difference now, then? On the 24th episode?
Gordon: Well, I honestly don't know. It seems to be something that's inherent with the gastro side of the hospital service. Most of Karen's other admissions have been to urology and we've never had this problem. And they've been really accommodating to Karen and made the stay as good as you can make a hospital stay. We're not asking for any more than that.
Host: I'm sure you've already heard this, well I'll read it out anyway. This comes from the NHS trust in question, which says that "patients with ME have a range of needs that often require complex multidisciplinary care. All treatment we provide to patients with ME is as closely in line with NICE guidance as possible. And ensuring that they have the best clinical care and experience, the best clinical outcomes remains the highest priority. We continue to work to provide care that will deliver the best outcome for our patients." What is the outcome currently?
Gordon: The outcome at the moment is very uncertain. I mean, Karen is in a dire and desperate situation and we're all very desperate. And we're very scared at the consequences and we're feeling extremely helpless to the point Karen now wants to discharge. And that discharge would mean no fluid, no feed at home, and you can only imagine where that would lead to.
Host: (quietly) Yeah.
Gordon: Karen has been denied suitable and appropriate healthcare quite simply. And we don't want to sort of challenge a hospital or come at loggerheads with a hospital; we just want to provide what is best for Karen, to make a really bad situation to a degree tolerable if that's the right sort of word. Because we've also been told (this is a quote from Karen actually) "They're making her life impossibly difficult in hosptial but they won't give her community care either." The community virtual ward service is saying they won't give IV fluid support on the community. So we can't be in hospital, we can't be at home. So we're just feeling totally helpless and isolated. And they are ignoring, despite what they say, they are ignoring the NICE guidelines, and they've also received advice from an expert specialist in severe ME and they're ignored that as well. And the expert said the same sorts of things. That they should be trying to provide a room and they should be allowing Heather to stay 24/7.
Host: Michael, I hear the frustration in your voice and I know you must be very tired as well. Because these things are very wearing. Let's see what happens. Please do keep in touch with us, and best wishes your family, and of course, to Karen. That is Karen Gordon's father, Michael Gordon.