Came across this study i.e. via Health Rising:
Frontier studies on fatigue, autonomic nerve dysfunction, and sleep-rhythm disorder
https://link.springer.com/article/10.1007/s12576-015-0399-y
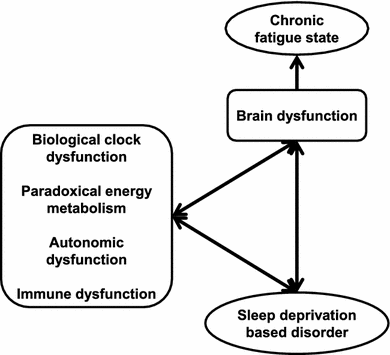
Role of sleep and circadian rhythm in fatigue recovery (Fig.
2)
Sleep features in individuals with CFS or chronic fatigue state
CFS is a medically unexplained disabling illness characterized by persistent relapsing fatigue of at least 6 months’ duration with low activity levels. Post-exertion malaise, neurocognitive dysfunction, infection-related symptoms, autonomic dysfunctions, and sleep disturbances are also major features of CFS.
Six studies reported no CFS specific findings in polysomnography (PSG) or actigraphy in contrast with CFS patients’ significant sleep complaints [
41–
46]. Fatigue or pain was well correlated with sleep disturbances and daily activity in patients with CFS or a CFS-related disorder, such as fibromyalgia [
43,
47–
49]. Interestingly, there was a weak correlation between fatigue score and sleepiness score in individuals without fatigue-related disorders [
50].
Under ambulatory monitoring conditions using home-based PSG or actigraphy, patients with CFS showed significant longer bedtime sleep, longer awake time after sleep onset, and less efficient sleep [
51–
55]. Individuals with CFS had a high incidence of undiagnosed primary sleep disorders [
56,
57]. This result strikes a note of warning for physicians.
Eight studies reported objective abnormalities in patients with CFS in terms of respiratory index, electroencephalographic power spectrum, and sleep-awake switching dynamics [
58–
65]. Gotts et al. showed that patients with CFS were divided into four clusters by sleep features based on hierarchical cluster analysis [66]. Those dynamics-based and cluster analysis results may reveal the heterogeneity of CFS pathophysiology and a new viewpoint regarding an analytical approach. It was also noted that total Pittsburgh sleep quality index score might not be suitable for patients with CFS [
67,
68]. There were no significant actigraphic or polysomnographic differences between patients with CFS and a control group [
49,
65,
68].
Fig. 2
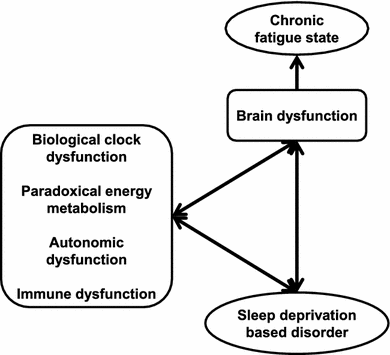
Chronic fatigue state induced by sleep deprivation. Accumulation of sleep deprivation caused brain dysfunction with/without biological dysfunctions. Fundamental biofunctions (biological clock, energy metabolism, autonomic activity, and immune system), sleep disorders, and brain functions interacted with each other and created negative chains. Chronic fatigue state was observed as the output of brain dysfunctions
Full size image
Font size reduced and paragraph breaks added.