Cerebral hypoperfusion in post-COVID-19 cognitively impaired subjects revealed by arterial spin labeling MRI
Ajčević, Miloš; Iscra, Katerina; Furlanis, Giovanni; Michelutti, Marco; Miladinović, Aleksandar; Buoite Stella, Alex; Ukmar, Maja; Cova, Maria Assunta; Accardo, Agostino; Manganotti, Paolo
Cognitive impairment is one of the most prevalent symptoms of post Severe Acute Respiratory Syndrome COronaVirus 2 (SARS-CoV-2) state, which is known as Long COVID. Advanced neuroimaging techniques may contribute to a better understanding of the pathophysiological brain changes and the underlying mechanisms in post-COVID-19 subjects.
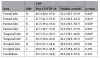
We aimed at investigating regional cerebral perfusion alterations in post-COVID-19 subjects who reported a subjective cognitive impairment after a mild SARS-CoV-2 infection, using a non-invasive Arterial Spin Labeling (ASL) MRI technique and analysis. Using MRI-ASL image processing, we investigated the brain perfusion alterations in 24 patients (53.0 ± 14.5 years, 15F/9M) with persistent cognitive complaints in the post COVID-19 period. Voxelwise and region-of-interest analyses were performed to identify statistically significant differences in cerebral blood flow (CBF) maps between post-COVID-19 patients, and age and sex matched healthy controls (54.8 ± 9.1 years, 13F/9M).
The results showed a significant hypoperfusion in a widespread cerebral network in the post-COVID-19 group, predominantly affecting the frontal cortex, as well as the parietal and temporal cortex, as identified by a non-parametric permutation testing (p < 0.05, FWE-corrected with TFCE). The hypoperfusion areas identified in the right hemisphere regions were more extensive.
These findings support the hypothesis of a large network dysfunction in post-COVID subjects with cognitive complaints. The non-invasive nature of the ASL-MRI method may play an important role in the monitoring and prognosis of post-COVID-19 subjects.
Link | PDF (Nature Scientific Reports)
Ajčević, Miloš; Iscra, Katerina; Furlanis, Giovanni; Michelutti, Marco; Miladinović, Aleksandar; Buoite Stella, Alex; Ukmar, Maja; Cova, Maria Assunta; Accardo, Agostino; Manganotti, Paolo
Cognitive impairment is one of the most prevalent symptoms of post Severe Acute Respiratory Syndrome COronaVirus 2 (SARS-CoV-2) state, which is known as Long COVID. Advanced neuroimaging techniques may contribute to a better understanding of the pathophysiological brain changes and the underlying mechanisms in post-COVID-19 subjects.
We aimed at investigating regional cerebral perfusion alterations in post-COVID-19 subjects who reported a subjective cognitive impairment after a mild SARS-CoV-2 infection, using a non-invasive Arterial Spin Labeling (ASL) MRI technique and analysis. Using MRI-ASL image processing, we investigated the brain perfusion alterations in 24 patients (53.0 ± 14.5 years, 15F/9M) with persistent cognitive complaints in the post COVID-19 period. Voxelwise and region-of-interest analyses were performed to identify statistically significant differences in cerebral blood flow (CBF) maps between post-COVID-19 patients, and age and sex matched healthy controls (54.8 ± 9.1 years, 13F/9M).
The results showed a significant hypoperfusion in a widespread cerebral network in the post-COVID-19 group, predominantly affecting the frontal cortex, as well as the parietal and temporal cortex, as identified by a non-parametric permutation testing (p < 0.05, FWE-corrected with TFCE). The hypoperfusion areas identified in the right hemisphere regions were more extensive.
These findings support the hypothesis of a large network dysfunction in post-COVID subjects with cognitive complaints. The non-invasive nature of the ASL-MRI method may play an important role in the monitoring and prognosis of post-COVID-19 subjects.
Link | PDF (Nature Scientific Reports)
Last edited: