Cheshire
Senior Member (Voting Rights)
Barbara Stussman1*, Ashley Williams2, Joseph Snow3, Angelique Gavin4, Remle Scott1,  Avindra Nath4 and Brian Walitt5
Avindra Nath4 and Brian Walitt5
Abstract
Background: Myalgic encephalomyelitis/chronic fatigue syndrome is characterized by persistent and disabling fatigue, exercise intolerance, cognitive difficulty, and musculoskeletal/joint pain. Post–exertional malaise is a worsening of these symptoms after a physical or mental exertion and is considered a central feature of the illness. Scant observations in the available literature provide qualitative assessments of post–exertional malaise in patients with myalgic encephalomyelitis/chronic fatigue syndrome. To enhance our understanding, a series of outpatient focus groups were convened.
Methods: Nine focus groups totaling 43 patients who reported being diagnosed with myalgic encephalomyelitis/chronic fatigue syndrome were held between November 2016 and August 2019. Focus groups queried post–exertional malaise in daily life and participants' retrospective memory of post–exertional malaise that followed an exercise provocation with a cardiopulmonary exercise test. Data analysis followed the grounded theory method to systematically code and categorize the data to find meaningful patterns. A qualitative software package was used to move text into categories during data coding.
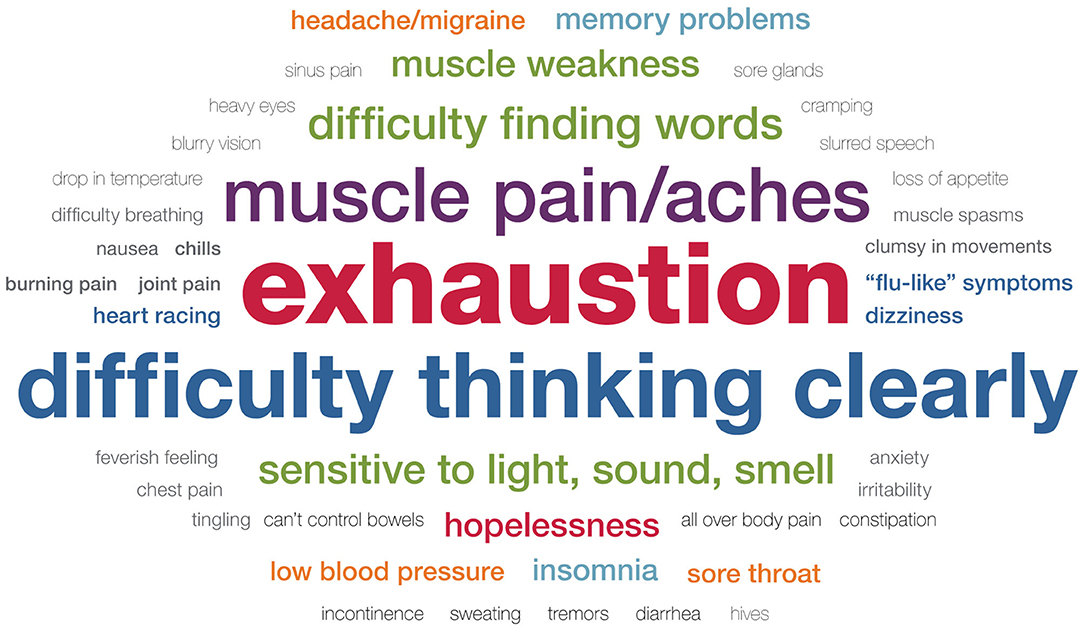
Results: A wide range of symptoms were attributed to exertion both in daily lives and following cardiopulmonary exercise testing. While three core symptoms emerged (exhaustion, cognitive difficulties, and neuromuscular complaints), participants' descriptions were notable for their unique individual variations. Of 18 participants who responded to questions centered around symptoms following a cardiopulmonary exercise test, 17 reported that symptoms started within 24 h and peaked in severity within 72 h following the cardiopulmonary exercise test. Patients described post–exertional malaise as interfering with their ability to lead a “normal” life.
Conclusion: The experience of post–exertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome varies greatly between individuals and leads to a diminished quality of life. myalgic encephalomyelitis/chronic fatigue syndrome patients describe post–exertional malaise as all-encompassing with symptoms affecting every part of the body, difficult to predict or manage, and requiring complete bedrest to fully or partially recover. Given the extensive variability in patients, further research identifying subtypes of post–exertional malaise could lead to better targeted therapeutic options.
https://www.frontiersin.org/articles/10.3389/fneur.2020.01025/full
 Avindra Nath4 and Brian Walitt5
Avindra Nath4 and Brian Walitt5Abstract
Background: Myalgic encephalomyelitis/chronic fatigue syndrome is characterized by persistent and disabling fatigue, exercise intolerance, cognitive difficulty, and musculoskeletal/joint pain. Post–exertional malaise is a worsening of these symptoms after a physical or mental exertion and is considered a central feature of the illness. Scant observations in the available literature provide qualitative assessments of post–exertional malaise in patients with myalgic encephalomyelitis/chronic fatigue syndrome. To enhance our understanding, a series of outpatient focus groups were convened.
Methods: Nine focus groups totaling 43 patients who reported being diagnosed with myalgic encephalomyelitis/chronic fatigue syndrome were held between November 2016 and August 2019. Focus groups queried post–exertional malaise in daily life and participants' retrospective memory of post–exertional malaise that followed an exercise provocation with a cardiopulmonary exercise test. Data analysis followed the grounded theory method to systematically code and categorize the data to find meaningful patterns. A qualitative software package was used to move text into categories during data coding.
Results: A wide range of symptoms were attributed to exertion both in daily lives and following cardiopulmonary exercise testing. While three core symptoms emerged (exhaustion, cognitive difficulties, and neuromuscular complaints), participants' descriptions were notable for their unique individual variations. Of 18 participants who responded to questions centered around symptoms following a cardiopulmonary exercise test, 17 reported that symptoms started within 24 h and peaked in severity within 72 h following the cardiopulmonary exercise test. Patients described post–exertional malaise as interfering with their ability to lead a “normal” life.
Conclusion: The experience of post–exertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome varies greatly between individuals and leads to a diminished quality of life. myalgic encephalomyelitis/chronic fatigue syndrome patients describe post–exertional malaise as all-encompassing with symptoms affecting every part of the body, difficult to predict or manage, and requiring complete bedrest to fully or partially recover. Given the extensive variability in patients, further research identifying subtypes of post–exertional malaise could lead to better targeted therapeutic options.
https://www.frontiersin.org/articles/10.3389/fneur.2020.01025/full
Last edited by a moderator: