Sorry to keep going on about this, but rereading it today has really made me cross.
Just taking the start of the abstract where they define PEM:
Background: Myalgic encephalomyelitis/chronic fatigue syndrome is characterized by persistent and disabling fatigue, exercise intolerance, cognitive difficulty, and musculoskeletal/joint pain. Post–exertional malaise is a worsening of these symptoms after a physical or mental exertion and is considered a central feature of the illness.
No. That's not a complete definition of ME, and it's not a good enough definition of PEM. It's closer to a definition of fatiguability. If that's what they thought they were researching, and designed the questions to elicit, they have failed.
This part worries me too and indicates why there was a problem with the study design I think.
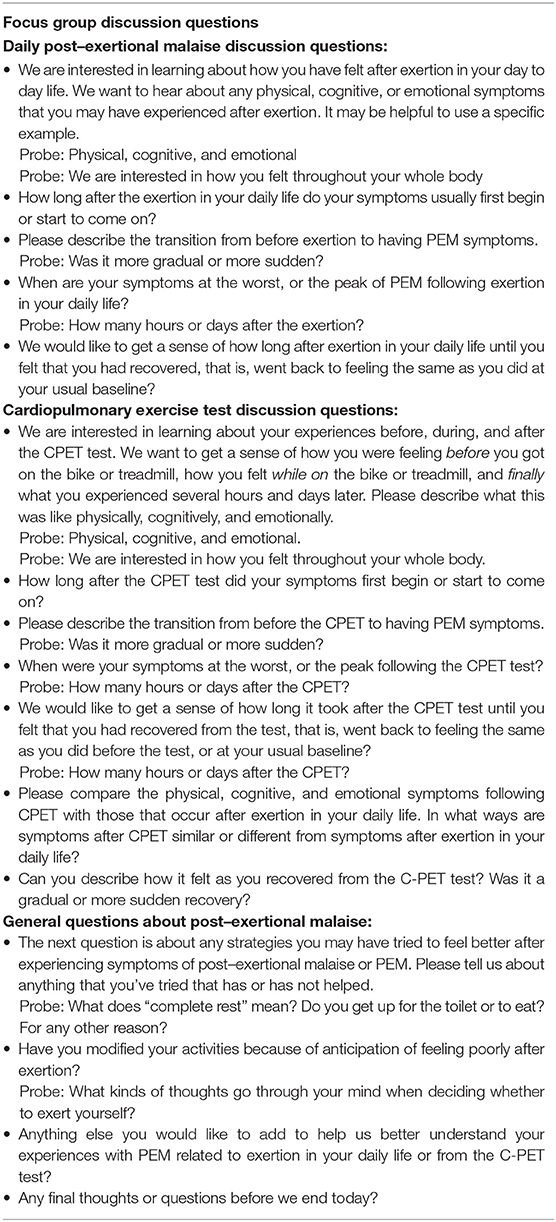
All focus groups were conducted by an experienced focus group moderator who had no prior experience with the study population or ME/CFS to ensure impartiality. The semistructured focus group script included broad questions aimed to explore patients' experiences of having PEM, both in their daily lives and in response to the CPET test. Discussion questions centered around activities that can trigger PEM, specific symptoms of PEM, how long after exertion symptoms began, how long the symptoms lasted, and at what point the symptoms were at their worst.
If the facilitator knows nothing about ME, how can they possibly understand why the questions asked didn't enable patients to differentiate between ME symptoms and the day to day effects of fatiguability while pacing successfully and not crashing, and the completely different (to me) major crash and loss of ability to continue pacing normally for a day or usually much longer and feeling very ill that I understand to be PEM.
The questions and prompts used in the focus groups:
https://www.frontiersin.org/files/A...11-01025-HTML/image_m/fneur-11-01025-t001.jpg
Look at the first set of questions. They are not about PEM, they about how you feel after any exertion in daily life. And the prompts include physical, cognitive and emotional 'exertion' so they are feeding the idea of emotion in from the start.
No wonder they ended up thinking a crash after a CPET was different from what they thought was PEM in normal life.
Sorry, I'll stop going on about this now. It's making me angry. Oooh dear, that's an emotion, maybe it will trigger PEM... (sarcasm).
I'd really like to hear what others think about my concern about this study. To me it's looking more and more like it was set up to find the set of answers they wanted to find, not to explore PEM in depth.