Ethics approval - or non-approval?
The ethics statement reads:
"Ethical approval.
Audit approval was provided by the Psychological Medicine Clinical Academic Group (ID number PPF191115) at the South London and Maudsley Hospital. All patients provided informed written."
Why did this not go to the REC? This is in effective part of the same group doing the research. Is this actually an audit approval for a service evaluation? Is this actually an ethics exemption reference?
@dave30th I'm hoping you could look into this since it sounds rather like another Crawley (school absence, National Outcomes Database / ALPASC) misdirection.
I would very much like to know what the "informed consent" statement was - and whether it was made clear this would be a widely distributed research publication rather than an internal or NHS only audit.
Given the 14 year period of collecting data, I find it highly unlikely that this research was planned at the start - it seems more likely that all accessing the service were asked to complete some kind of consent form for data collection that was required and also included a tick box referring to future unspecified research. I wonder if data may have been used that was collected prior to consent.
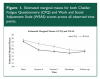
Fatigue got significantly worse after 4 weeks - see figure 1. Chalder Fatigue Scale was the only fatigue measure reported separately.
Wessely hasn't "retired" from CFS research then
Data collection continued up until 2018. No mention of Wessely stopping work on this at any time, which is unusual in research.
Perhaps the "retirement" has been reversed due to his apparent need to be involved in whatever research money may be available for long covid and chronic fatigue after the coronavirus. Or perhaps it's a desperate need to get some of the limelight.
Chronic Fatigue is redefined
Fatigue was redefined as mental OR physical. But chronic fatigue is always described as physical and possibly mental / cognitive as well. Including by the NHS which describes "tiredness". Mental fatigue in the absence of other symptoms is actually
cognitive dysfunction or cognitive fatigue. Or brain fog. Not chronic fatigue.
"...67 (7%) reporting either physical or mental fatigue."
That's not consistent with the
NHS definition currently in use.
NHS definition
insists on additional symptoms so Oxford criteria alone is excluded since it may not have extra symptoms.
Dropouts - or deaths?
There is no information on how follow up was done and if GPs were contacted to ask patients (who may have moved) if they wished to complete questionnaires - or even if they were still alive. This is pretty standard and may I think have been done in the PACE trial or other BPS trials.
This trial "dropouts" may been deaths. A FOIA request already exists showing NHS England and Wales records ME related deaths *every year*.
No baseline data
I can't understand how a study can be allowed to include those without baseline data. An improvement between week 7 and the end, or week 4 and the end doesn't tell us whether patients improved. overall
Inventing the data
There are standard, well known methods for accounting for missing data, none were used. They simply invented what was missing using a man average. There is no actual statement to indicate if removing those without complete data would affect the results. It's particularly a concern with high numbers of baseline AND follow up data missing.
Completion - actually under 30%?
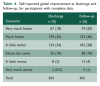
Looking at the tables, no questionnaire was completed by over 300, so each measure relied on only a third of the people in the trial.
Non-completion of forms may be because people were simply too ill to attend OR too ill to both have a conversion / appt and complete the form - so any points of non-completition may represent deterioration.
Patients actually got worse
Figure 1 demonstrates that if it works out does so within the first 4 weeks, and after that patients go steadily downhill. The trial report claim that improvements were maintained is 1. untrue for the length of the trial, 2. untrue for end of treatment compared to follow up, 3. only statistically insignificant deterioration happened between end of treatment and follow up.
Anyone requested the full anonymised data?
I think analysing only completed, and only those with baseline would show non-completion was by those most ill at the end or most ill at the start.
Do those who do more sessions (20) do worse than those that do 7 or 4? If the 4 sessions are most effective, as shown in the data, then what topics are covered? If sessions 1-4 are pacing, diet, finding a baseline and 5-7 or 20 are increasing activity, ignoring symptoms, etc then this would actually show pacing works but not not the CBM model.
A standard formula for missing data may give very different results.
I suspect median and mean analysis would give very different results since the CFS doesn't reflect those getting worse from treatment and may be reflecting a few who got significantly better.
Medication
I presume some started medication - why is there no record of how many and how they fared after? Especially pain and sleep medication or anti-depressants for sleep.
Chronic fatigue actually got worse - And Worse on 2 of the 3 scores
See Figure 1 - Both CFQ and WSAS show worse scores and CFQ was the only measure of fatigue alone.
SP-36 includes many other factors - it's possible that patients only improved on non-physical measures but improved enough for an overall improvement.
(Taken from APA):
"The SF-36 assesses eight health concepts:
- limitations in Quality of life physical activities because of health problems;
- limitations in social activities because of physical or emotional problems;
- limitations in usual role activities because of physical health problems);
- bodily pain;
- general mental health (psychological distress and well-being);
- limitations in usual role activities because of emotional problems;
- vitality (energy and fatigue); and
- general health perceptions"
with only 4 of 8 SP-36 measures concerning physical health I think this may explain why fatigue and work status got worse but SF-36 improved.
Patient harm
Not reported. Wonder if any had hospitalizations, suicide attempts, self-harm, A&E attendance or developed new mental health problems (or relapsed). GPs would not inform services but *might* be required to alert
Reasons for dropouts
Not given. Were they asked?
A statistically anonymous of patient info is under this heading.
Complaints received by the service
None mentioned. According to the comment on Dave Tuller's blog at least one complaint was ignored and wrongly described as a "therapy session" and remained unresolved. That's malpractice.