The authors gave a presentation about their findings on the NMCB meeting a couple of days ago. I've made a brief summary of the talk on social media:
1) Dr. Felipe Correa da Silva shared more info about the first 10 brain autopsies from the Netherlands. In this new thread, we made a brief summary of his presentation.
2) The Netherlands Brain Bank has 40 years of experience. Their ME/CFS program started in April 2024. They currently have 61 registrations and the aim is to have 200 by the end of their 5-year project.
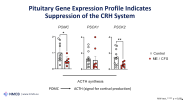
3) They already did 10 autopsies but aim to do 50 over a period of ten years. They submitted a manuscript on their first findings titled “Hypothalamic-pituitary-adrenal axis dysfunction in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome”.
4) Below is a graph of their main result. They found an almost depletion of Corticotropin-Releasing Hormone (CRH-ir) neurons in the brains of ME/CFS patients.

5) Correa da Silva said they looked at the HPA axis because low cortisol has been linked to ME/CFS symptoms. But: “The magnitude of the changes in the brains of people with ME seem to be very high, much more than we expected initially.”
6) They also found a down-regulated expression of genes related to CRH signalling and lower cortisol levels in the cerebrospinal fluid.
7) CRH is the key that starts the Hypothalamic-Pituitary-Adrenal (HPA) axis, the body’s primary stress response system. It goes something like this: Hypothalamus -> CRH -> Pituitary gland -> ACTH -> Adrenal glands -> Cortisol.
8 ) Lots of ME/CFS patients also have sleep disturbances, so the authors were also interested in orexin, a neuropeptide that keeps us awake and is disrupted in nacrolepsy. They plan to look at this more closely but preliminary results also suggest a decrease in ME/CFS.
9) The second talk of the presentation wasn't about the HPA axis or stress system but about microglia, the immune cells in the brain.
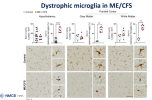
10) Correa da Silva explains: "something that was striking for us, is that we did not observe more microglia as we would expect in a neuro-inflammatory condition where there is infiltration of microglia..."
11) Instead, they saw that the microglia are dystrophic: they are fragmented. The cell body is not connected to the processes and the processes are also fragmented in itself.
12) This is a somewhat new histological feature. Not a lot of people in the world have described it. There’s no harmonized system to quantify this yet but they certainly see it in the brains of ME/CFS patients.
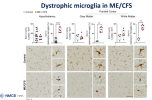
13) This was not only in the hypothalamus, but something that seems to be a widespread effect, in both gray and white matter.
14) The authors also looked at HLA which acts as a proxy for microglia activation and this showed no clear effect. They also found no evidence of abnormal T (CD3) or B (CD79a) cell presence in the central nervous system of ME/CFS patients.
15) Correa da Silva described the findings as follows: "So in the patients that donate their brains, possibly endstage patients, we do not see signs of classical neuro-inflammation, but we see dystrophic, rather senescent microglia."
16) "ME/CFS has been thought to be a neuro-inflammatory throughout the whole disorder but this might not be true. It might be that after a certain point the neuro-inflammation stops because the cells are senescent and cannot keep up with their continuous activation."
17) One extra interesting finding is that in the Hypothalamus (the PVN) they found increased CD68 positive microglia. CD68 is a protein found on the membrane of lysosomes so this points to increased phagocytosis (clean-up) and possibly micro-enviromental injury.

18) In other parts of the brain such as the the parietal cortex, they do not see that. So it seems to be triggered by local events, rather than a widespread mechanism.
19) So what's next? The researchers plan to also look at mitochondria-related changes and use other tools than histopathology. They got another grant for single cell transcriptomics (snRNA-seq) of 3 regions: the hypothalamus, frontal cortex and hippocampus.
20) The full presentation of Dr. Felipe Correa da Silva at the NMCB meeting can be watched here:
https://www.youtube.com/watch?v=30DkFAXHjDI