Summary
Mast cell activation syndrome (MCAS) is a rare condition that is characterised by recurrent sudden-onset episodes of severe systemic symptoms associated with the release of mast cell mediators. In many cases the recurrent episodes present as anaphylaxis.
Acute episodes of MCAS-associated anaphylaxis must be managed according to the usual emergency protocol, with immediate administration of intramuscular adrenaline (epinephrine) alongside an ABCDE approach to assess the need for supplemental oxygen, intravenous fluids, and airway management.
A diagnosis of MCAS is confirmed by evidence of a significant rise in a mast cell marker (e.g., serum tryptase) during acute episodes and a positive clinical response to a medication that targets a mast cell mediator. It is important to then evaluate the MCAS sub-type: primary (clonal), secondary (usually associated with IgE-dependent allergy), or idiopathic.
Treatment involves trigger identification and avoidance together with a stepwise approach to long-term pharmacotherapy, starting with an antihistamine (H1 antagonist) and H2 antagonist. Add-on options include a leukotriene receptor antagonist, sodium cromoglicate, and omalizumab. Patients with refractory primary (clonal) MCAS may require cytoreductive therapy. Lifelong immunotherapy is recommended for individuals with sensitivity to Hymenoptera venom.
Definition
MCAS is a rare condition defined by severe, episodic reactions to mast cell-derived mediators.
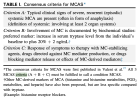
[1] For a diagnosis of MCAS to be confirmed:
[2][3]
- There must be recurrent, acute episodes of symptoms/signs associated with secreted mast cell mediators that affect two or more organ systems at the same time
- A transient rise in a mast cell mediator (e.g., tryptase) must be confirmed during these acute episodes, and
- The symptoms must respond to drugs that either target released mast cell mediators or suppress mast cell activation (e.g., antihistamine, H2 antagonist, leukotriene receptor antagonist, sodium cromoglicate).
In most cases, MCAS presents with recurrent episodes of anaphylaxis.
[4]