http://www.londonhp.nhs.uk/wp-content/uploads/2011/03/MUS-whole-systems-approach.pdf
Medically Unexplained Symptoms (MUS)
A whole systems approach
July 2009 – December 2010
Page 20
"It may be possible within the new polyclinic model that the routine of psychologists working
with consultants would develop. Equally, they could work in hospitals in more structured ways
such as a ‘pelvic pain’ clinic.
"We would suggest that one consultant in each department should lead on this area of the
work, helping other consultants to think about difficult presentations, ensuring patients can
access the psychologist appropriately and reviewing the care of patients where no biological
explanation can be found. At present, patients are referred back to primary care or on to
another secondary care department, thus allowing the clinician to maintain the idea that
medically unexplained symptoms are not part of their work.
"It will be necessary for acute clinicians working in these clinics to code patients that they feel
may have MUS. There are often no codes available to do this in these specialities. We would
advise therefore that the ICD codes F44, F45 and F48 are used as ‘catch-all’ codes. These
would include any situation where the clinicians felt there was an element of MUS affecting the
patient and their management. This is necessary in order for outcomes to be quantifiable.
These codes are to be used to monitor outcomes; clinicians can use the codes where
appropriate, in conjunction with other codes."
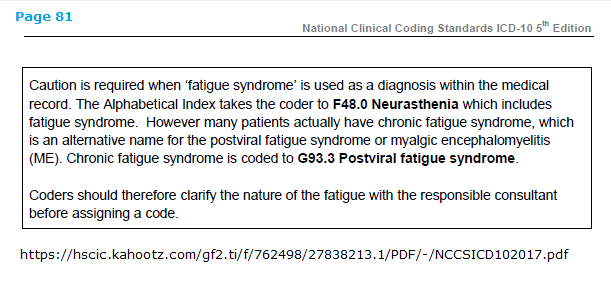
Note that under
F48.0 Neurasthenia (and its inclusion:
Fatigue syndrome) there is an exclusion (
Excl.) for G93.3.
Also note:
But there are no exclusions for G93.3 under the ICD-10 F45.x codes.
So an additional F45.x diagnosis can be added to an existing or new diagnosis of G93.3, or to any other disease or condition.
"F45 Somatoform disorders
"The main feature is repeated presentation of physical symptoms together with persistent requests for medical investigations, in spite of repeated negative findings and reassurances by doctors that the symptoms have no physical basis. If any physical disorders are present, they do not explain the nature and extent of the symptoms or the distress and preoccupation of the patient."
Compare this with
Bodily distress disorder for ICD-11, which replaces most of the ICD-10
Somatoform disorder categories and also subsumes and replaces
F48.0 Neurasthenia.
A patient may be diagnosed with BDD, or an additional diagnosis of BDD can be added in the presence of a general medical condition or disease.
"...If another health condition is causing or contributing to the symptoms, the degree of attention is clearly excessive in relation to its nature and progression."
Contrary to Dr Diane O'Leary's contention that:
"Criteria* for BDD are not particularly problematic for ME patients. They are compatible with construing ME as a biological disease" [1]
BDD is
very problematic and I have continued to push for exclusions for the ICD-11 8E49 terms.
*NB: There are no "criteria" as such for ICD-11's BDD but a disorder description and characterization text, which allows clinicians more flexibility to use clinical judgement when assessing whether a patient meets the required features and disorder description than the more rigid DSM-5
Somatic symptom disorder (SSD) criteria set and thus poses an even greater threat to patients with chronic, multiple symptoms.
1 “BODILY STRESS SYNDROME” INFO SHEET, March 2018, Dr Diane O'Leary for Forward-ME:
http://www.forward-me.org.uk/Reports/BODILY STRESS SYNDROME INFO SHEET CORRECTED.pdf