“When I Lie in the Dark, Rage Overcomes Me”
A Life Before the Darkness
Before her illness, Natascha S. was a lively young woman who loved music, dancing, and traveling. She studied in Göttingen, worked with young refugees in Leipzig, and was surrounded by a close circle of friends. At 29, her life changed abruptly when she developed ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome). Now 31, she lives isolated in a darkened 15-square-meter room, entirely dependent on others for care.
Life in a Darkened Room
Natascha’s world is almost completely sealed off from light and sound. Her windows are taped shut, and anyone entering must wear an FFP2 mask and speak only in whispers. She cannot sit up, stand, or speak for long. Her daily existence revolves around pain management, rest, and survival. For the past 14 months, she has been bedridden. “I feel buried alive,” she whispers. She can no longer watch films, listen to music, or make phone calls. Every small act of independence—using a spoon, washing, communicating—is an exhausting effort.
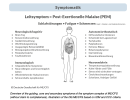
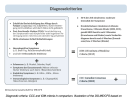
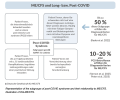
The Invisible Disease
ME/CFS is a chronic, multisystem illness that can follow viral infections such as Epstein-Barr or Covid-19. It causes severe fatigue, pain, and hypersensitivity to stimuli. Germany has an estimated 650,000 patients, though many remain undiagnosed. Despite being classified by the WHO since 1969, ME/CFS is still poorly understood and under-researched. For those severely affected, even minimal exertion can cause a “crash”—a period of extreme worsening known as Post-Exertional Malaise. Natascha experiences these repeatedly.
Fighting Through the Pain
Because communication can trigger a crash, Natascha speaks in short whispers or via hand signals. To conduct interviews, she takes small doses of Tavor, a sedative that allows brief relief from pain. She cannot work, and her finances are strained; her family and friends support her through donations and care. “I’m trapped in my body,” she says quietly. Yet her will to live persists. Anger—at the system, at the neglect—is what keeps her alive.
Writing as Resistance
Unable to undergo therapy, Natascha turns to writing. On her Instagram account, she documents her illness and criticizes medical neglect and social discrimination. “When I lie in the dark, rage overcomes me,” she wrote once. Her activism has reached politicians, including former Health Minister Karl Lauterbach, who admitted systemic failures in ME/CFS care. For Natascha, writing is both emotional survival and political protest—an attempt to change the system from her bed.
Friendship and Survival
When her condition collapsed in 2024, friends Sophie and Axel became her full-time caregivers for three weeks. They fed, washed, and monitored her through sleepless nights, terrified she might die. Medical professionals often dismissed her condition as psychological. Their experience revealed the extent of institutional ignorance. Eventually, Natascha’s mother took over her care, and a small team of assistants now supports her daily needs. Each helper was chosen for understanding the political dimension of illness and disability.
Holding On to Small Joys
Despite constant pain, Natascha still finds fleeting beauty: the sound of rain, a bird’s call, the presence of a friend’s dog beside her bed. She dreams of having an assistance dog and, one day, enough strength to sit in a wheelchair again. Her friends describe her as astonishingly resilient, though the fear of losing her is constant. “I still have so much desire for life,” she whispers, even as she keeps the paperwork for assisted suicide near her bed—unfilled, but present.
Endurance in the Dark
Natascha’s story is one of isolation, friendship, and quiet defiance. She lives between exhaustion and anger, despair and hope. Her body confines her, but her words reach beyond the dark room. “How many more years can I endure this?” she asks. Yet she continues—alive, alert, and fighting for recognition, dignity, and the right to be seen.