Hi Suzy,
Again, I'm so glad you take time to answer my questions.
You are welcome.
I see that WHO's defjnition is slightly different than the general definition of "synonym" in that they saý they cannot be used interchangeably. Thanks for this!
Note that the WHO's unmodified ICD-10 does not include Synonyms, per se, in the Tabular List. In the Tabular List, ICD-10 lists the Title category, any inclusions to the Title category and any exclusions. There may be associated or alternative terms in the Index which point to the Title code.
So, for example, in the unmodified ICD-10, we have PVFS as the Title category, with BME listed as its inclusion. CFS is in the Index, where it points to the G93.3 code.
WHO says this about ICD-10 Index terms:
According to a February 2009 response from WHO HQ Classifications, Terminology and Standards Team, terms that are listed in the Index may be:
a synonym to the label (title) of a category of ICD;
a sub-entity to the disease in the title of a category;
or a “best coding guess”
The Introduction to
ICD-10 Volume 3: The Alphabetical Index Version for 2006 lists several possible relationships between a term included in the Alphabetical Index and a term included in the Tabular List to which it is indexed:
“The terms included in the category of the Tabular List are not exhaustive; they serve as examples of the content of the category or as indicators of its extent and limits. The Index, on the other hand, is intended to include most of the diagnostic terms currently in use. Nevertheless, reference should always be made back to the Tabular List and its notes, as well as the guidelines provided in Volume 2, to ensure that the code given by the Index fits with the information provided by a particular record.
“Because of its exhaustive nature, the Index inevitably includes many imprecise and undesirable terms. Since these terms are still occasionally encountered on medical records, coders need an indication of their assignment in the classification, even if this is to a rubric for residual or ill-defined conditions. The presence of a term in this volume, therefore, should not be taken as implying approval of its usage.”
In indexing
Chronic fatigue syndrome to G93.3, ICD-10 does not specify whether it views the term as a synonym, a sub-entity or “best coding guess” to
Postviral fatigue syndrome or to
Benign myalgic encephalomyelitis. Nor does ICD-10 specify how it views the relationship between
Postviral fatigue syndrome and
Benign myalgic encephalomyelitis.
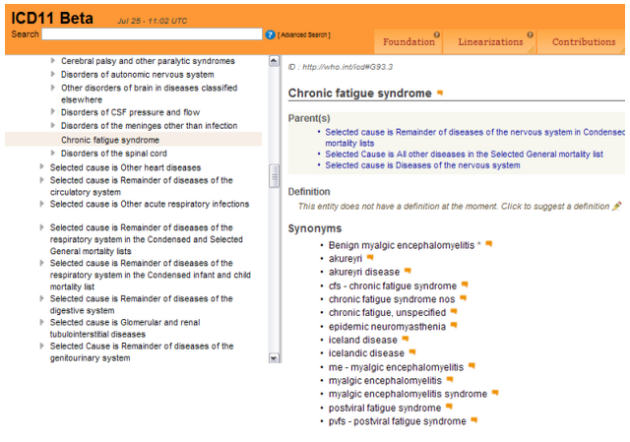
The structure of ICD-11 is far more complex than ICD-10 and will contains, potentially, more information about category terms, set out according to the ICD-11 "Content Model". Category terms in ICD-11 are listed hierarchically and a coded for term may have one or more coded for "child" categories or "grandchildren" sitting beneath it.
There will be a Title concept term; its parent class or classes (if it is listed under one or more parents or under more than one chapter, which is permissible for ICD-11); a Definition/Description text (although many of these texts are not yet completed); it will list any specified inclusion terms (under "Inclusions", in the Foundation linearisation and at the top of the Synonyms list, in the MMS linearisation); there may be a list of "Narrower terms"; then a list of any Exclusions. Some category terms have even more information included.
Additional terms listed under Synonyms and Index terms may be alternative clinical terms, terms more commonly used by patients, or historical terms that are now rarely used.
ICD-11 includes terms like "charley-horse" under index terms which is a colloquial U.S. term for muscle cramps.
For example, for ICD-11, the current listing for PVFS, has PVFS as the
Title concept term. CFS and BME are both specified under
Inclusions and take the same code as PVFS:
https://icd.who.int/dev11/l-m/en#/http://id.who.int/icd/entity/569175314
Currently the list of Synonym terms (which are also listed as Index terms) is:
- akureyri
- akureyri disease
- CFS - [chronic fatigue syndrome]
- chronic fatigue, unspecified
- epidemic neuromyasthenia
- iceland disease
- icelandic disease
- myalgic encephalomyelitis
- myalgic encephalomyelitis syndrome
- ME - [myalgic encephalomyelitis]
- PVFS - [postviral fatigue syndrome]
I wonder if it was more reasonable to drop the term "CFS" completely. I understand that there exists fatigue, most often as a symptom of other diseases, and I'll include inflammation in general to that. But most doctors know close to nothing. I fear, at least in Germany, doctors will diagnose "CFS" instead of ME due to simplicity, ignorance, laziness and misinformation from officials (e.g. DEGAM); most doctors haven't heard about ME, but some about CFS. They will do symptom picking or symptom invention (my experiences) and then it's CFS. E.g. they simply ignored my PEM/PENE experiences, invented and picked symptoms et voilà! Depression!
Whilst both Mary and I do not like the CFS term, we had to be realistic in our proposals. Given that in 2013, ICD Revision were considering making CFS the Title term, we did not feel they would give any consideration to retiring the CFS term, altogether.
The following extract isn't from the proposal's rationale text but from a Q & A I prepared about the proposal and it sets out our rationale for not requesting that the CFS term is retired:
Q1: Your proposal for ICD-11 does not recommend retiring CFS. Why is that?
A: Realistically, CFS cannot be retired from the classification at this time.
Some patients and advocates have expressed concerns that our proposal does not recommend
retirement of CFS. We share concerns about the CFS term.
However, realistically, chronic fatigue syndrome cannot be removed from ICD at this time
because the term will continue to be used clinically, is required for social security, insurance and
reimbursement and will still be included in other globally used electronic health record systems.
For example, chronic fatigue syndrome is specified as the preferred concept term in SNOMED CT
International Edition and its National Extensions. ICD-11 has been designed to link with SNOMED
CT and the cross mapping between the two terminology systems is in preparation.
If ICD Revision could be persuaded to retire the term, the owners of SMOMED CT would need to
be convinced, too. SNOMED CT is used in over 80 countries. As mentioned in Q5, SNOMED CT
will be adopted in the UK for NHS primary care use by 2018, replacing the Read Codes (CTV3)
terminology system and is scheduled for implementation across all NHS clinical settings by 2020.
Since ICD Revision was proposing between 2010-2013 that CFS should be elevated to the lead
(or "concept title") term, and in the absence of any alternative consensus proposals from the
work group since early 2013, we considered it unlikely that a strong enough case for retiring the
term, at this point, could be built.
Unlike the U.S.'s ICD-10-CM, ICD-11 won't implement, globally, on a specific date – it will be a
staggered and lengthy adoption process.
Over a hundred countries use ICD-10, including countries licensed by WHO to develop national
modifications, like Canada, the U.S. and Germany, which already have CFS in their Tabular Lists.
WHO requires statistical comparability between one ICD edition to another for data analysis.
During the transition period (which will span several years and potentially longer, in the case of
Canada and the U.S.), statistics will continue to be collected using ICD-10 alongside data using
the new version, until the majority of Member States have implemented the new edition.
Given these considerations, we consider there is a strong possibility that ICD Revision
would reject outright any submission that includes a proposal for the retirement of the
CFS term, during the early years of the transition process where data collected from
two editions will be aggregated for analyses.
At some future point, scientific advances will hopefully provide robust evidence to support a case
for retirement of the CFS term and/or for relocation of ME to another chapter, or for parenting
ME under multiple chapters, or for creation of a specific parent class for ME, at which point, new
proposals can be submitted via the annual update and revision process.
ICD Revision's, Dr Christopher Chute, wrote to me, on February 22: "What is produced say in
2018 will continue to evolve, ICD11 is designed for graceful evolution. It may differ in
substantial ways by the time the first country implements it, say 5-6 years from now from what
is put forth in 2018."
There was uncertainty around ICD Revision's intentions for the three legacy terms while we were
drafting our proposal and that uncertainty continues. Given the March 30 deadline for submission
of proposals for potential inclusion in the initial 2018 release, the absence of any proposals from
the work group and the non disclosure of the WHO classification experts' and Joint Task Force's
position on these terms, it was considered strategically preferable to propose what we felt stood
a chance of consideration than to submit recommendations we felt risked outright rejection.