Sly Saint
Senior Member (Voting Rights)
Relationship between Cardiopulmonary, Mitochondrial and Autonomic Nervous System Function Improvement after an Individualised Activity Programme upon Chronic Fatigue Syndrome Patients
Katarzyna Buszko
Sławomir Kujawski
Jo Cossington
Joanna Słomko
Monika Zawadka-Kunikowska
Małgorzata Tafil-Klawe
Jacek J. Klawe
Djordje G. Jakovljevic
Mariusz Kozakiewicz
Karl J. Morten
Helen Dawes
James W. L. Strong
Modra Murovska
Jessica Van Oosterwijck
Fernando Estevez-Lopez
Julia L. Newton
Lynette Hodges
Paweł Zalewski
on behalf of the European Network on ME/CFS (EUROMENE)
Abstract
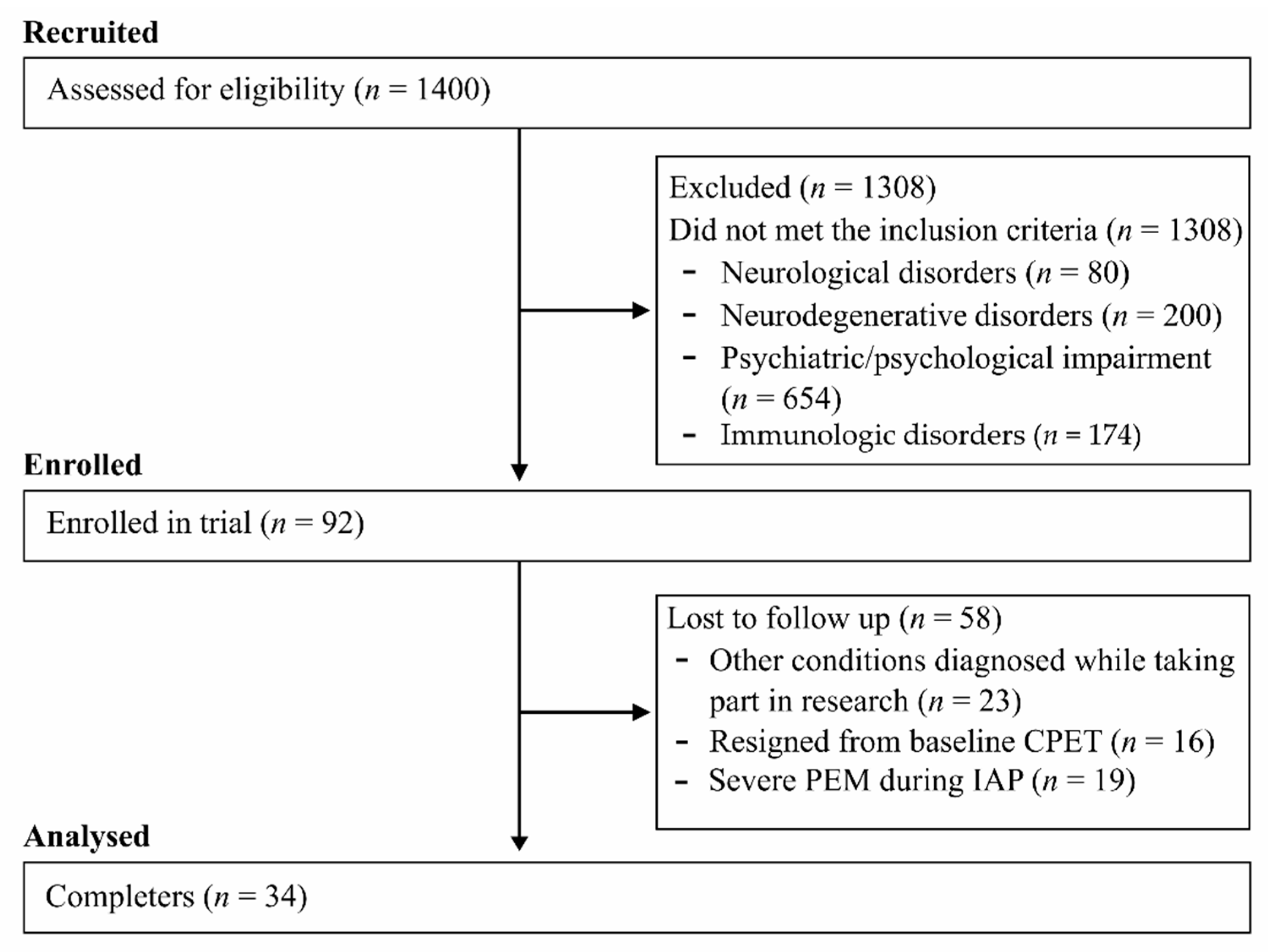
Background: The therapeutic effects of exercise from structured activity programmes have recently been questioned; as a result, this study examines the impact of an Individualised Activity Program (IAP) on the relationship with cardiovascular, mitochondrial and fatigue parameters.
Methods: Chronic fatigue syndrome (CFS) patients were assessed using Chalder Fatigue Questionnaire (CFQ), Fatigue Severity Score (FSS) and the Fatigue Impact Scale (FIS). VO2peak, VO2submax and heart rate (HR) were assessed using cardiopulmonary exercise testing. Mfn1 and Mfn2 levels in plasma were assessed.
A Task Force Monitor was used to assess ANS functioning in supine rest and in response to the Head-Up Tilt Test (HUTT).
Results: Thirty-four patients completed 16 weeks of the IAP. The CFQ, FSS and FIS scores decreased significantly along with a significant increase in Mfn1 and Mfn2 levels (p = 0.002 and p = 0.00005, respectively). The relationships between VO2 peak and Mfn1 increase in response to IAP (p = 0.03) and between VO2 at anaerobic threshold and ANS response to the HUTT (p = 0.03) were noted.
Conclusions: It is concluded that IAP reduces fatigue and improves functional performance along with changes in autonomic and mitochondrial function. However, caution must be applied as exercise was not well tolerated by 51% of patients.
https://www.mdpi.com/2077-0383/10/7/1542
Katarzyna Buszko
Sławomir Kujawski
Jo Cossington
Joanna Słomko
Monika Zawadka-Kunikowska
Małgorzata Tafil-Klawe
Jacek J. Klawe
Djordje G. Jakovljevic
Mariusz Kozakiewicz
Karl J. Morten
Helen Dawes
James W. L. Strong
Modra Murovska
Jessica Van Oosterwijck
Fernando Estevez-Lopez
Julia L. Newton
Lynette Hodges
Paweł Zalewski
on behalf of the European Network on ME/CFS (EUROMENE)
Abstract
Background: The therapeutic effects of exercise from structured activity programmes have recently been questioned; as a result, this study examines the impact of an Individualised Activity Program (IAP) on the relationship with cardiovascular, mitochondrial and fatigue parameters.
Methods: Chronic fatigue syndrome (CFS) patients were assessed using Chalder Fatigue Questionnaire (CFQ), Fatigue Severity Score (FSS) and the Fatigue Impact Scale (FIS). VO2peak, VO2submax and heart rate (HR) were assessed using cardiopulmonary exercise testing. Mfn1 and Mfn2 levels in plasma were assessed.
A Task Force Monitor was used to assess ANS functioning in supine rest and in response to the Head-Up Tilt Test (HUTT).
Results: Thirty-four patients completed 16 weeks of the IAP. The CFQ, FSS and FIS scores decreased significantly along with a significant increase in Mfn1 and Mfn2 levels (p = 0.002 and p = 0.00005, respectively). The relationships between VO2 peak and Mfn1 increase in response to IAP (p = 0.03) and between VO2 at anaerobic threshold and ANS response to the HUTT (p = 0.03) were noted.
Conclusions: It is concluded that IAP reduces fatigue and improves functional performance along with changes in autonomic and mitochondrial function. However, caution must be applied as exercise was not well tolerated by 51% of patients.
https://www.mdpi.com/2077-0383/10/7/1542
Last edited: