- Home
- Forums
- Discussion topics
- Causes, Epidemiology, Criteria, Naming discussions
- Possible causes and predisposing factor discussion
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
The symptom signaling theory of ME/CFS involving neurons and their synapses
- Thread starter ME/CFS Science Blog
- Start date
Yann04
Senior Member (Voting Rights)
I dont think so. It’s spread to other toes and when i treat it it pops up on different toes.Ingrown nail?
I wonder if anyone has checked for muscle activity in resting PWME. I'm imagining some signals causing the muscle cells to contract randomly; enough to qualify as exercise, but not enough firing together to move limbs noticeably.But I have no idea if pwME/CFS have more muscles than other similarly inactive people that can still use the muscles.
Too difficult to measure important factors in living brains. Also, brains are very complex, so there are a lot of potential factors involved. Furthermore, the abnormalities could be limited to just a few brain cells, and the measurable factors could be limited in range and time frame. Imagine that the difference between mild ME and severe is just a few molecules in vesicles moving micrometers (nanometers?) between brain cells, leaving no trace even a few micrometers away. Astrocytes stick processes into synapse gaps, but do we know what actual molecular transfers are occurring and what's normal or abnormal?why are we not seeing anything?
The abnormalities might not exist post-mortem, and measuring them in live brains might be bad for live brains, at least with present technology.
Hoopoe
Senior Member (Voting Rights)
But isn't that a peripheral neuropathy, one that wouldn't explain any of the core ME/CFS symptoms?
And why would a injury that is not severe cause much more debilitating fatigue symptoms than the severe CNS injuries that are already known?
If it is possible, it will probably have this special connection with the neural pathway that produces symptoms, so we're back to where we started.
A peripheral neuropathy could be described as exaggerated/false/distorted signals reaching the brain.
When I spent time visiting SFN forums, it was obvious a portion of patients had PEM and could easily meet diagnostic criteria for ME/CFS. But the general sentiment was that ME/CFS was something to take distance from, because it was mysterious and subjective, while SFN was more real and could be supported by a biopsy.
I hope one day we will understand how all this fits together.
Last edited:
Verity
Senior Member (Voting Rights)
This sounds plausible to me from an experience standpoint. In a crash, I sometimes feel like I can’t fully relax my muscles at rest.I wonder if anyone has checked for muscle activity in resting PWME. I'm imagining some signals causing the muscle cells to contract randomly; enough to qualify as exercise, but not enough firing together to move limbs noticeably.
Yeah, i always thought is was something damaged in the brain to do with sleep because i have never made much improvement over 20 years. But how the symptom PEM would fit into that is a confusing worry.Re. orexin. It is a neuropeptide. There are over 100 known neuropeptides in the human brain and the expectation is that more will be discovered.
Since they affect so many different things, including sensory perception, regulation of the vascular system, metabolism, sleep, they seem potentially relevant to ME/CFS. I remember leptin has come up before in ME/CFS, although this was in relation to its peripheral role.
someUsername
Established Member
Does Cyclo somehow could influence a neurological issue? Or does this theory imply that Cyclo could not have actually worked?
Snow Leopard
Senior Member (Voting Rights)
Yes, I mixed up CNS with neurological in general.But isn't that a peripheral neuropathy, one that wouldn't explain any of the core ME/CFS symptoms?
And why would a injury that is not severe cause much more debilitating fatigue symptoms than the severe CNS injuries that are already known?
The issue isn't merely the injury, but the response to that injury. Eg nerve sensitisation.
The brain receiving out of wack autonomic or fatigue signals can have explanatory power. The fact that ME/CFS like syndromes are common post-GBS should give pause for thought.
Autopsies of severe ME/CFS patients HAVE revealed DRG neuropathy so it is a viable hypothesis.
What is not quite clear to me about a neurological hypothesis: Why are these problems apparently more common after glandular fever? How does EBV seemingly have more influence on synapses or neurons than other viral infections?
If we accept a comparison to something like a "ongoing sickness response", then I see no reason to also not see a similarity to the PVF that EBV causes in many people, but why is EBV particularly good at doing that?
This is a good question. EBV and other herpesviruses are known to infect peripheral nerves and can sometimes be found in cerebral-spinal fluid too.
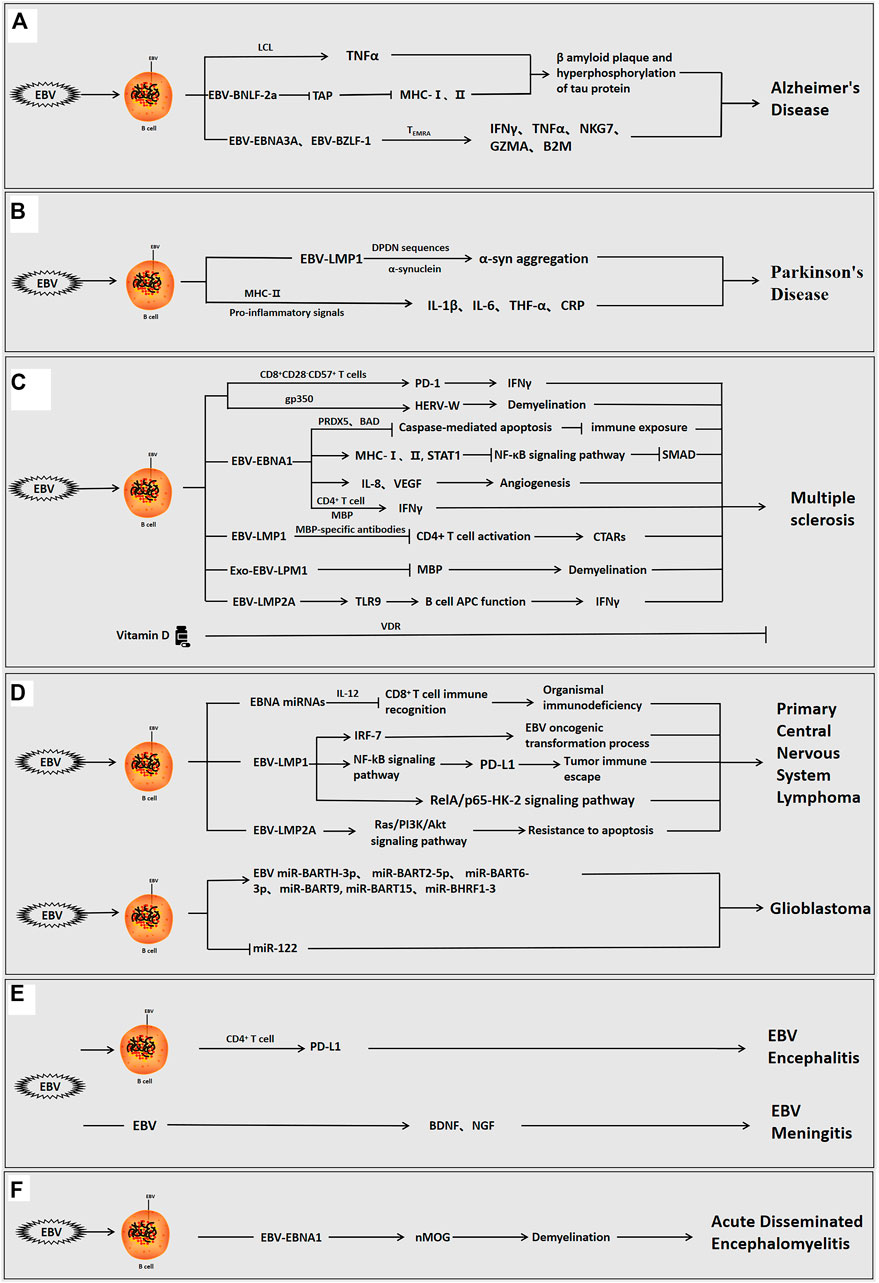
Frontiers | Epstein-Barr Virus and Neurological Diseases
Epstein-Barr virus (EBV), also known as human herpesvirus 4,is a double-stranded DNA virus that is ubiquitous in 90-95% of the population as a gamma herpesv...
The herpes viruses and particularly EBV are far more complex than other viruses, having *far* more genes than most viruses at about 85 allowing for much more complex behaviour.
Sure, but then they would be very unfamiliar with how ME/CFS patients usually present.
But I have no idea if pwME/CFS have more muscles than other similarly inactive people that can still use the muscles.
Your body adjusts to the intensity of activity over the week, rather than the quantity. You can easily go backwards in fitness when doing 10,000 steps per day if it reduces your intensity peaks.
Last edited:
Jonathan Edwards
Senior Member (Voting Rights)
Does Cyclo somehow could influence a neurological issue?
Cyclophosphamide could kill T lymphocytes in brain but is unlikely to affect brain cells otherwise.
However, if a brain problem is dependent on background signals from normal levels of immune activity from either B or T cells it might be affected.
ME/CFS Science Blog
Senior Member (Voting Rights)
Regarding neuronal damage, there's this paper from last year that reported (slightly) increased Neurofilament Light Chain.
Trial Report - Plasma Neurofilament Light Chain: A Potential Biomarker for Neurological Dysfunction in ME/CFS, 2024, Azcue et al | Science for ME
This has also been reported in Long Covid en fibromyalgia.:
Long COVID: plasma levels of neurofilament light chain in mild COVID-19 patients with neurocognitive symptoms | Molecular Psychiatry
Plasma neurofilament light chain in fibromyalgia: A case control study exploring correlation with clinical and cognitive features - Ruggieri - 2025 - European Journal of Pain - Wiley Online Library
Trial Report - Plasma Neurofilament Light Chain: A Potential Biomarker for Neurological Dysfunction in ME/CFS, 2024, Azcue et al | Science for ME
This has also been reported in Long Covid en fibromyalgia.:
Long COVID: plasma levels of neurofilament light chain in mild COVID-19 patients with neurocognitive symptoms | Molecular Psychiatry
Plasma neurofilament light chain in fibromyalgia: A case control study exploring correlation with clinical and cognitive features - Ruggieri - 2025 - European Journal of Pain - Wiley Online Library
Verity
Senior Member (Voting Rights)
Lots of conditions cause exercise intolerance. Not all exercise intolerance is PEM. I’m wary of conflating something that lacks one of the main features of PEM with what you see in ME.Dr. Sarah Schafer has discussed how some/many Sjogren's patients (which can cause both peripheral neuropathy as well as CNS involvement) seem to have a flavor of PEM, though she feels that it differs from the PEM in ME/CFS in lacking the delayed onset and the possibility of leading to enduring declines in baseline seen in ME/CFS.
nataliezzz
Senior Member (Voting Rights)
Yes, for sure. I think the kind of thing she is describing in Sjogren's patients seems to be a bit different from what would typically be considered "exercise intolerance" or transient PESE though (e.g. see her description of hers below... can be triggered by sensory input, giving a presentation leads to extended decline, etc.), though as I said it may be distinguished from the PEM of ME/CFS by lack of delayed onset and possibility of leading to more enduring declines in baseline. Like I said, I suspect that kind of PEM is probably unique to ME/CFS (& possibly some cases of CCI).Lots of conditions cause exercise intolerance. Not all exercise intolerance is PEM. I’m wary of conflating something that lacks one of the main features of PEM with what you see in ME.
Yann04
Senior Member (Voting Rights)
I think something similar is experienced with acute illness as well. Like if you do too much when you have the flu.
What seems to really seperate ME is the duration of PEM and fact sometimes you never get back to baseline. I’m strongly in favour of making sure definitions of PEM are strict on this. Because I think it could do a lot of damage to give transient worsenings the same name as what can be permament in ME/CFs.
What seems to really seperate ME is the duration of PEM and fact sometimes you never get back to baseline. I’m strongly in favour of making sure definitions of PEM are strict on this. Because I think it could do a lot of damage to give transient worsenings the same name as what can be permament in ME/CFs.
poetinsf
Senior Member (Voting Rights)
Neuroimmune activation in TBS is a rather well-established fact. One could question whether that is the cause of post-concussion fatigue. But neuroimmune activation is also a rather well established as a cause of fatigue, such as age-related fatigue. (https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2017.00208/full)Many people with post-concussion syndrome suffer from something akin to PEM and I don't think anybody has any idea on what the cause of post-concussion syndrome is.
I don't know what is something akin to PEM. But I don't remember PEM being mentioned in any personal account for post-concussion fatigue I've read. if PEM is a part of post-concussion fatigue, it apparently is not as prominent as in ME/CFS.
I remember we had discussed this before. Here is an old post on it to not derail this thread: https://www.s4me.info/threads/traum...ces-to-me-cfs-including-pem.24965/post-597559.Neuroimmune activation in TBS is a rather well-established fact. One could question whether that is the cause of post-concussion fatigue. But neuroimmune activation is also a rather well established as a cause of fatigue, such as age-related fatigue. (https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2017.00208/full)
I don't know what is something akin to PEM. But I don't remember PEM being mentioned in any personal account for post-concussion fatigue I've read. if PEM is a part of post-concussion fatigue, it apparently is not as prominent as in ME/CFS.
poetinsf
Senior Member (Voting Rights)
Thanks, I'm glad you have a better memory than mine. It appears we both have been very consistent on this topic!I remember we had discussed this before. Here is an old post on it to not derail this thread: https://www.s4me.info/threads/traum...ces-to-me-cfs-including-pem.24965/post-597559.
Some posts have been moved to a thread about Upper Airway Resistance Syndrome (UARS) and a PEM discussion thread.
What if ME/CFS is an impaired ability to turn off excitatory neural circuits (or alternatively, inappropriate activation of these circuits)?
I was watching an Intro to Neuroscience lecture, where the teacher described different kinds of micro neural circuits (at 24:30). There are positive feedback, negative feedback, and other little neuron networks.
I'm imagining various types of "exertion", whether physical or mental, trigger some types of excitatory neurons. A positive feedback loop starts that keeps them active.
In healthy people, soon after the exertion ends, the circuit would be "turned off". For some reason, in ME/CFS, it stays on.
How does this fit the symptoms?
The "wired", "adrenaline-like", or insomnia symptoms that begin shortly after exertion:
This would be the excitatory neurons just continuing to fire far longer than needed, maintaining a state of alertness.
Delayed fatigue and other symptoms:
After a while of the neurons firing for too long, the circuit is finally turned off. Maybe the mechanism that is meant to turn it off kicks in very late.
Maybe something like a drug tolerance mechanism happens, like in stimulant (cocaine, amphetamine, etc) withdrawal. The neurons are continually firing inappropriately, spewing out too many neurotransmitters, so other parts of the brain eventually notice and inhibit the circuits, become less sensitive to the neurotransmitters, or both. As in drug withdrawal, the crash is worse than baseline.
I was watching an Intro to Neuroscience lecture, where the teacher described different kinds of micro neural circuits (at 24:30). There are positive feedback, negative feedback, and other little neuron networks.
I'm imagining various types of "exertion", whether physical or mental, trigger some types of excitatory neurons. A positive feedback loop starts that keeps them active.
In healthy people, soon after the exertion ends, the circuit would be "turned off". For some reason, in ME/CFS, it stays on.
How does this fit the symptoms?
The "wired", "adrenaline-like", or insomnia symptoms that begin shortly after exertion:
This would be the excitatory neurons just continuing to fire far longer than needed, maintaining a state of alertness.
Delayed fatigue and other symptoms:
After a while of the neurons firing for too long, the circuit is finally turned off. Maybe the mechanism that is meant to turn it off kicks in very late.
Maybe something like a drug tolerance mechanism happens, like in stimulant (cocaine, amphetamine, etc) withdrawal. The neurons are continually firing inappropriately, spewing out too many neurotransmitters, so other parts of the brain eventually notice and inhibit the circuits, become less sensitive to the neurotransmitters, or both. As in drug withdrawal, the crash is worse than baseline.
Last edited:
Yann04
Senior Member (Voting Rights)
I have to say this is starting to look quite convincing to me. Atleast I can start really seeing myself as potentially having the theoretical disease you describe.What if ME/CFS is an impaired ability to turn off excitatory neural circuits (or alternatively, inappropriate activation of these circuits)?
I was watching an Intro to Neuroscience lecture, where the teacher described different kinds of micro neural circuits (at 24:30). There are positive feedback, negative feedback, and other little neuron networks.
I'm imagining various types of "exertion", whether physical or mental, trigger some types of excitatory neurons. A positive feedback loop starts that keeps them active.
In healthy people, soon after the exertion ends, the circuit would be "turned off". For some reason, in ME/CFS, it stays on.
How does this fit the symptoms?
The "wired", "adrenaline-like", or insomnia symptoms that begin shortly after exertion:
This would be the excitatory neurons just continuing to fire far longer than needed, maintaining a state of alertness.
Delayed fatigue and other symptoms:
After a while of the neurons firing for too long, the circuit is finally turned off. Maybe the mechanism that is meant to turn it off kicks in very late.
Maybe something like a drug tolerance mechanism happens, like in stimulant (cocaine, amphetamine, etc) withdrawal. The neurons are continually firing inappropriately, spewing out too many neurotransmitters, so other parts of the brain eventually notice and inhibit the circuits, become less sensitive to the neurotransmitters, or both. As in drug withdrawal, the crash is worse than baseline.
