What about pregnancy? I remember a thread where some members reported remission during pregnancy.
Pregnancy can influence many of the things that are proposed to be part of the ME/CFS puzzle, like blood flow, in addition to hormones and the immune system.
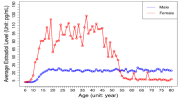
On the peaks - the ages also coincide with times in life where you might have less time to rest and have more activities in your life that’s not necessarily for you to control. Time where what was up until then a manageable «I need more rest» situation into rolling PEM and eventually not being able to take part in things anymore.
For children:
In Norway, you have different times in childcare. Ages 1-2/3 will have opportunities to rest during the day, but this diminishes as the child becomes older and has to follow along with the group where most don’t need a daily nap. It has become increasingly common to have extracurricular activities even for ages 2+ in addition to childcare.
Starting school is obviously also a big change in a child’s life, and there are yet more extracurricular activities.
Moving from the younger classes to the older ones (we have a split between 1-4, 5-7 and 8-10, which for some may require a change in school environment. For me it meant going from a 10 min walk to school to a 30+min busdrive with all the noise that follows being in a bus full of children going to school). The older ages sometimes have more homework, but this can differ a lot between schools.
Schoolyears 11-13 are voluntary, but in practice required. Recently more focus has been put on attendance (I would bot have been able to finish school with todays rules).
Adults:
University years in Norway can allow for being sick for years without getting a diagnosis. We have student loans that you can have for years (you need something from a doctor to not be told you’re lagging too far behind to continue, but it is still a time where it can be possible to muddle along with illness pretty well. A sad joke in my disability community is that many master student’s over here really ought to be on disability instead of getting student loans…)
After university (or in stead of university) you might be working and have various possibilities to rest. But if you become a parent (currently this typically happens in early 30s in Norway), that doesn’t hold anymore. Your typical child in Norway starts in childcare around ~1 year old, and from then on is believed to bring home 5-10 infections a year during childcare for the parents to deal with.
It can just be too much even without any additional hormonal issues.
Time of diagnosis/time of symptom onset may also be very difficult to assess properly. I’ve thought I developed ME after I outgrew my migraines as a child, but with covid causing migraines - was my migraines actually post viral and then it for some reason changed into ME? My migraine triggers are now my PEM triggers so to me it doesn’t feel too far fetched.