arewenearlythereyet
Senior Member (Voting Rights)
Thank you for taking the time to reply and to provide more detail on your views on the disease.thanks, once again, for constructive remarks.
Fatigue is a subjective feeling which is extremely hard to objectivate. Exhaustion, lactic acid accumulation, sleep disturbance etc. can be measured, but the feeling of fatigue can only be estimated by using questionnaires. Patients expressing that they were clearly less tired, and could resume their activity, and in whom the FSS was decreased by at least 15%, were considered responders. If the subjective feeling of fatigue was decreased, but the FSS was not, or vice versa, they were considered non-responders.
Again I insist on the fact that the nutriceutical (food supplement containing vitamins, amino acids, minerals and plant extracts with medical application, in French called ALICAMENTS) are not to be confounded with homeopathy. The effect of several of such nutriceuticals has been proven for the treatment of e.g. male infertility, migraine, metabolic syndrome, hyperlipaemia, and benign prostate hyperplasia. For each of these conditions, specific mixtures of ingredients are being used. I have published the results of trials with these nutriceuticals, both open-label trials and placebo controlled studies. Several of these studies add biological "surrogate markers" to the clinical findings, whenever possible.
I repeat that the prime purpose of treating patients with fatigue is to make them feel better, to increase their "energy" so that they can resume their "normal" professional and familiy life, albeit often with limitations. In general, this is the purpose of medicine.
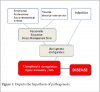
Now, giving insulin to patients suffering of diabetes does not cure their disease, but improves their health and quality of life. Giving the nutriceutical I have used DOES NOT CURE ME/CFS, but it interferes with (one of) the probable pathogenetic mechanisms, improving the quality of life of a proportion of them. Since the nutriceutical is not toxic and causes no adverse effects, the benefit over risk ratio is positive. Also, the basic ethical rule "first do not harm" (primum non nocere, Hippocrates of Kos, MD, 460-377 BC) is honoured.
Regarding poor studies SUCH as PACE etc. I like to refer to my publication in attachment.
I am a retired professor of internal medicine, endocrinology and metabolic diseases, having published approximately 700 scientific papers, and lectured at 400 congresses and symposia over the world. I have been teaching at Ghent Univesity for 40 years and have personnaly treated several tenthousands of patients. I have organised several multicentre trials in my function of steering committe member of the World Health Organisation. I know the limitations of the present paper, which I clearly mention. So, once again, read the paper for what it contains, and not more nor less.
I think context is definitely key in terms of claims associated with any nutritional supplement.
I personally take many of these and have got some improvements in symptoms from things like B vitamins and mitochondrial support supplements. However I would say that the use of these are mainly around symptom relief to improve quality of life while I'm sick.
These treatments haven't moved me forward in terms of improving my capability, they have just eased things like brain fog, and reduced the duration of PEM episodes slightly. I am pretty certain that my energy envelope hasn't increased since I've been measuring heart rate activity and steps before and during taking the supplements.
It's really important to stress that this is for symptom relief/ quality of life rather than to give people more energy and feeling less fatigued which could be misleading to many desperate sufferers who are looking for a "cure"particularly with the confusion around the name ( as you mention in your paper).
That is why I hope with future studies you might include the wider aspects of the disease and perhaps use activity and cognitive measurements. It would also be good to see if people's energy envelope did increase or whether it remains unchanged with measures such as constant heart rate monitoring to give an objective measure of activity before and after supplementation. This would also show up PEM episodes so the frequency of these vs activity could then be also captured? I also found that initial supplementation took a while to settle down (6-8 weeks) and in the case of B12 this took a long time (6 months). Longer term studies would be helpful to see what is going on in terms of continuous supplemental therapy. It's also worth noting that pacing activity in a lot of cases will control a lot of symptoms without supplementation so this would need to be a control.
I hope you find these critiques useful and hope you will post some more of your findings.