This article has been retracted, see post #31.
----------------------------------------------------------
Causal Relationship Between Diet, Lipids, Immune Cells, and Chronic Fatigue Syndrome: A Two-Mediation Mendelian Randomization Study
Jixu Li, Qi Qin, Yiran Zhu, Yulu Qian, Jialu Yin, Xin Gao, Huijuan Wen, Pei Wang
[Line breaks added]
Abstract
Chronic fatigue syndrome (CFS) is a disorder characterized by severe unexplained fatigue and is associated with various factors including infections, immune responses, genetics, and environmental influences. However, the underlying mechanisms and possible interventions for CFS remain unclear. We used a two-mediated MR method to investigate causal relationships between diet, lipid levels, immune cells, and CFS.
Our findings suggest that certain lipids, specifically low-density cholesterol, apolipoprotein E, and apolipoprotein B, contribute to CFS development. Conversely, high-density lipoprotein cholesterol and apolipoprotein A1 may delay the onset of the syndrome.
Additionally, we explored how lipids affect fatigue through immune cell mediation. Factors, such as hematopoietic stem cell absolute count, the percentage of CD3-natural killer lymphocytes, and IgD presence on IgD+ CD38+ B cells may mediate the causal pathway linking lipids to CFS.
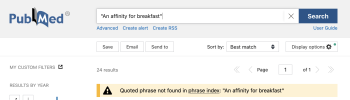
Furthermore, we examined the relationship between diet, lipids, and CFS. This indicated that specific dietary selections, like alcohol intake, a preference for chili peppers, and an affinity for breakfast, contributed to CFS. Conversely, cheese and pork consumption were protective factors against CFS. The protective effect of cheese consumption on CFS was mediated by apolipoprotein A1 and high-density lipoprotein cholesterol.
In conclusion, the study established an ecological chain: cheese consumption leads to increased high-density lipoprotein cholesterol and alters immune cell phenotypes—specifically, increasing the percentage of CD3-lymphocytes and IgD on IgD+ CD38+ B cells—ultimately influencing the development of CFS.
These findings enhance our understanding of how lipid levels and immune factors are related to CFS and how dietary choices can potentially mitigate the syndrome.
Link | PDF (Food Science & Nutrition) [Open Access]
----------------------------------------------------------
Causal Relationship Between Diet, Lipids, Immune Cells, and Chronic Fatigue Syndrome: A Two-Mediation Mendelian Randomization Study
Jixu Li, Qi Qin, Yiran Zhu, Yulu Qian, Jialu Yin, Xin Gao, Huijuan Wen, Pei Wang
[Line breaks added]
Abstract
Chronic fatigue syndrome (CFS) is a disorder characterized by severe unexplained fatigue and is associated with various factors including infections, immune responses, genetics, and environmental influences. However, the underlying mechanisms and possible interventions for CFS remain unclear. We used a two-mediated MR method to investigate causal relationships between diet, lipid levels, immune cells, and CFS.
Our findings suggest that certain lipids, specifically low-density cholesterol, apolipoprotein E, and apolipoprotein B, contribute to CFS development. Conversely, high-density lipoprotein cholesterol and apolipoprotein A1 may delay the onset of the syndrome.
Additionally, we explored how lipids affect fatigue through immune cell mediation. Factors, such as hematopoietic stem cell absolute count, the percentage of CD3-natural killer lymphocytes, and IgD presence on IgD+ CD38+ B cells may mediate the causal pathway linking lipids to CFS.
Furthermore, we examined the relationship between diet, lipids, and CFS. This indicated that specific dietary selections, like alcohol intake, a preference for chili peppers, and an affinity for breakfast, contributed to CFS. Conversely, cheese and pork consumption were protective factors against CFS. The protective effect of cheese consumption on CFS was mediated by apolipoprotein A1 and high-density lipoprotein cholesterol.
In conclusion, the study established an ecological chain: cheese consumption leads to increased high-density lipoprotein cholesterol and alters immune cell phenotypes—specifically, increasing the percentage of CD3-lymphocytes and IgD on IgD+ CD38+ B cells—ultimately influencing the development of CFS.
These findings enhance our understanding of how lipid levels and immune factors are related to CFS and how dietary choices can potentially mitigate the syndrome.
Link | PDF (Food Science & Nutrition) [Open Access]
Last edited: