rvallee
Senior Member (Voting Rights)
https://www.mdpi.com/2073-4409/10/2/386
Abstract
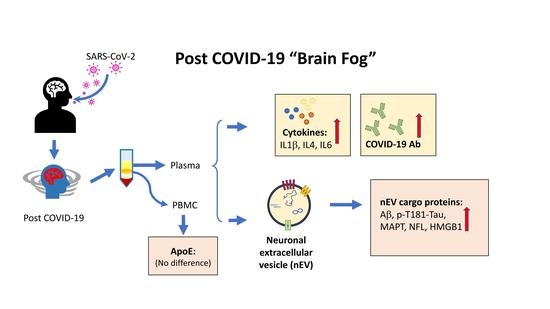
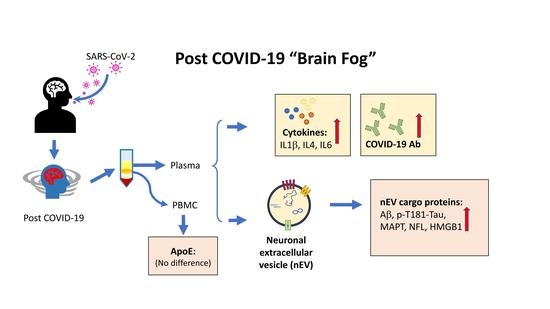
Not sure how informative but this image is included as a graphical abstract:
Abstract
As the SARS-CoV-2 pandemic continues, reports have demonstrated neurologic sequelae following COVID-19 recovery. Mechanisms to explain long-term neurological sequelae are unknown and need to be identified. Plasma from 24 individuals recovering from COVID-19 at 1 to 3 months after initial infection were collected for cytokine and antibody levels and neuronal-enriched extracellular vesicle (nEV) protein cargo analyses. Plasma cytokine IL-4 was increased in all COVID-19 participants. Volunteers with self-reported neurological problems (nCoV, n = 8) had a positive correlation of IL6 with age or severity of the sequalae, at least one co-morbidity and increased SARS-CoV-2 antibody compared to those COVID-19 individuals without neurological issues (CoV, n = 16). Protein markers of neuronal dysfunction including amyloid beta, neurofilament light, neurogranin, total tau, and p-T181-tau were all significantly increased in the nEVs of all participants recovering from COVID-19 compared to historic controls. This study suggests ongoing peripheral and neuroinflammation after COVID-19 infection that may influence neurological sequelae by altering nEV proteins. Individuals recovering from COVID-19 may have occult neural damage while those with demonstrative neurological symptoms additionally had more severe infection. Longitudinal studies to monitor plasma biomarkers and nEV cargo are warranted to assess persistent neurodegeneration and systemic effects.
Not sure how informative but this image is included as a graphical abstract: