boolybooly
Senior Member (Voting Rights)
"ACE2, Much More Than Just a Receptor for SARS-COV-2."
URL=https://www.frontiersin.org/article/10.3389/fcimb.2020.00317
Just came across this and thought of this thread.
I am still trying to make sense of it all but as I am understanding it... through a thick headache...
Given the nature of NO, its reduction in the experiment linked in the OP would imply some kind of ongoing inflammatory process in ME, if it proves replicable.
We dont know if it is AngII doing this but AngII also has this effect and is famous because of COVID as it is antagonistic to the product of ACE2 (which is Ang1-7) and may be implicated in COVID pathology (as the virus binds to ACE2 to enter cells).
So I would guess this finding might attract a little extra attention for that reason.
I still think replication is the first priority but would hope people would be more likely to try that because of the interest in COVID research.
URL=https://www.frontiersin.org/article/10.3389/fcimb.2020.00317
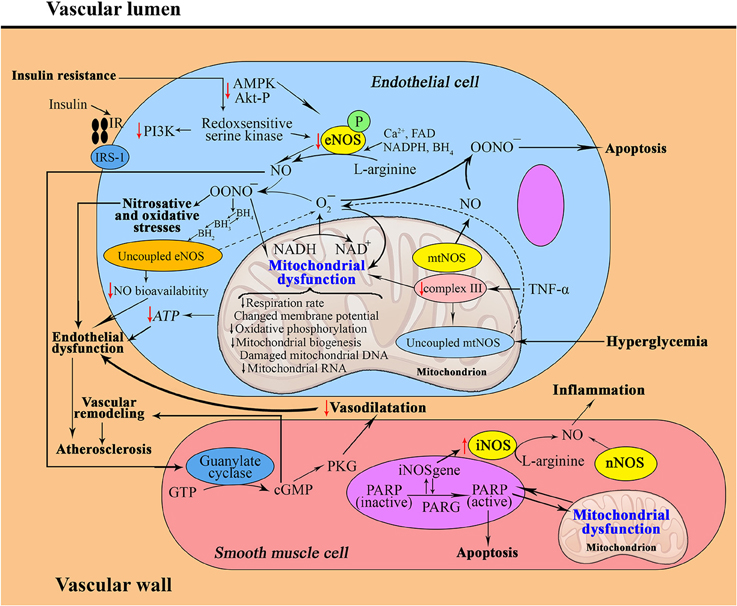
Ang II activates neutrophils and macrophages flux to the affected tissues and inhibits the production of nitric oxide
Just came across this and thought of this thread.
I am still trying to make sense of it all but as I am understanding it... through a thick headache...
Given the nature of NO, its reduction in the experiment linked in the OP would imply some kind of ongoing inflammatory process in ME, if it proves replicable.
We dont know if it is AngII doing this but AngII also has this effect and is famous because of COVID as it is antagonistic to the product of ACE2 (which is Ang1-7) and may be implicated in COVID pathology (as the virus binds to ACE2 to enter cells).
So I would guess this finding might attract a little extra attention for that reason.
I still think replication is the first priority but would hope people would be more likely to try that because of the interest in COVID research.