nataliezzz
Senior Member (Voting Rights)
Fibromyalgia in obstructive sleep apnea-hypopnea syndrome: a systematic review and meta-analysis
Jie He, Meifeng Chen, Na Huang, and Bo Wang
https://pmc.ncbi.nlm.nih.gov/articles/PMC11144865/
Abstract
Introduction: Fibromyalgia (FM) is a common condition in patients with obstructive sleep apnea-hypopnea syndrome (OSAHS). This meta-analysis aimed to evaluate differences in sleep monitoring indicators between patients with OSAHS and positive FM and patients with OSAHS and negative FM and to determine the incidence of FM in patients with OSAHS.
Methods: An exhaustive literature review was conducted to analyze the incidence of FM in patients with OSAHS, using online databases, including PubMed, EMBASE, Web of Science, CNKI, and Wanfang, both in English and Chinese. The quality of the included studies was assessed by two researchers using the Newcastle−Ottawa Scale scores. The acquired data were analyzed using Stata 11.0 software. Continuous variables were combined and analyzed using the weighted mean difference as the effect size. Conjoint analyses were performed using random-effects (I2 > 50%) or fixed-effect (I2 ≤ 50%) models based on I2 values.
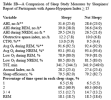
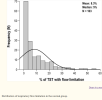
Results: Fourteen studies met the inclusion criteria. This study showed that 21% of patients with OSAHS experienced FM. Subgroup analyses were performed based on race, age, sex, body mass index, and diagnostic criteria for patients with OSAHS. These findings indicate that obese patients with OSAHS have a higher risk of FM, similar to females with OSAHS. Regarding most sleep monitoring indicators, there were no discernible differences between patients with OSAHS with positive FM and those with negative FM. However, patients with positive FM had marginally lower minimum arterial oxygen saturation levels than those with negative FM. The current literature suggests that patients with OSAHS have a high incidence of FM (21%), and FM has little effect on polysomnographic indicators of OSAHS.
Jie He, Meifeng Chen, Na Huang, and Bo Wang
https://pmc.ncbi.nlm.nih.gov/articles/PMC11144865/
Abstract
Introduction: Fibromyalgia (FM) is a common condition in patients with obstructive sleep apnea-hypopnea syndrome (OSAHS). This meta-analysis aimed to evaluate differences in sleep monitoring indicators between patients with OSAHS and positive FM and patients with OSAHS and negative FM and to determine the incidence of FM in patients with OSAHS.
Methods: An exhaustive literature review was conducted to analyze the incidence of FM in patients with OSAHS, using online databases, including PubMed, EMBASE, Web of Science, CNKI, and Wanfang, both in English and Chinese. The quality of the included studies was assessed by two researchers using the Newcastle−Ottawa Scale scores. The acquired data were analyzed using Stata 11.0 software. Continuous variables were combined and analyzed using the weighted mean difference as the effect size. Conjoint analyses were performed using random-effects (I2 > 50%) or fixed-effect (I2 ≤ 50%) models based on I2 values.
Results: Fourteen studies met the inclusion criteria. This study showed that 21% of patients with OSAHS experienced FM. Subgroup analyses were performed based on race, age, sex, body mass index, and diagnostic criteria for patients with OSAHS. These findings indicate that obese patients with OSAHS have a higher risk of FM, similar to females with OSAHS. Regarding most sleep monitoring indicators, there were no discernible differences between patients with OSAHS with positive FM and those with negative FM. However, patients with positive FM had marginally lower minimum arterial oxygen saturation levels than those with negative FM. The current literature suggests that patients with OSAHS have a high incidence of FM (21%), and FM has little effect on polysomnographic indicators of OSAHS.
Last edited by a moderator: