Small question. By who's authority do we accept the term MUS? Is it some official medical term that is used across medical specialties?
The reason I ask is that I wonder if it could be lobbied for the term pre-clinical symptoms. This has been my experience over many decades of illness. A particular vague symptom starts on it's own with no way of identifying what it might be about. Then years later it forms part of a now constellation of symptoms that crystalize into a known illness with an identifiable marker.
It's like medicine expects that when you walk in the illness has just come on full blown like days earlier you were the picture of health.
In the UK, the mandatory classification and terminology systems for use in NHS clinical settings are:
WHO's ICD-10 (Version 2015)
SNOMED CT UK Edition
SNOMED CT's terminology Concept codes are mapped to ICD-10 codes for interoperability.
There is no specific term for
Medically unexplained symptoms in ICD-10, in the "clinical modifications" of ICD-10 or in the forthcoming ICD-11.
The ICD-10 PHC (
The Diagnostic and Management Guidelines for Mental Disorders in Primary Care: ICD-10 Chapter V Primary Care Version), was published in 1996. It was intended as a simplified guideline to 25 "common mental disorders" developed as a diagnostic tool for use by practitioners without psychiatric training, by non medically trained health workers, for use in training, in low resource settings, low- to middle-income countries etc. NB: The guideline consists of only 25* mental disorders ie. there are no other abridged ICD-10 chapters for general medical conditions.
*There are circa 450 mental and behavioural disorders classified within Chapter V of ICD-10.
In the ICD-10 PHC, there is an
F45 Unexplained somatic complaints category, which corresponds to ICD-10's
F45 Somatoform disorders block. The ICD-10 PHC F45 category is more recently referred to by the chair of the working group that had developed the publication as "medically unexplained symptoms."
Unlike ICD-10 (and eventually ICD-11) the ICD-10 PHC publication is not mandatory for use by WHO member states. ICD-10 PHC has been under revision for ICD-11 PHC, for which 27 "common mental disorders" are proposed to be included. WHO has published no ETA for its completion and release.
For ICD-11 PHC,
Bodily stress syndrome (BSS) is proposed to replace the ICD-10 PHC categories: F45
Unexplained somatic complaints (also referred to as
"medically unexplained symptoms"); and F48
Neurasthenia. The
Bodily stress syndrome (BSS) disorder construct is being developed by the WHO, advised by an external
Primary Care Consultation Group (PCCG) (which again is chaired by emeritus Prof, Sir David Goldberg, who is now in his mid 80s). This is a different working group to the working group that developed the SSD-like,
Bodily distress disorder (BDD) that is going forward for the main ICD-11 classification. The PCCG is proposing a differently conceptualized disorder construct for ICD-11 PHC to the construct being used for the main ICD-11, which captures a different patient population.
The WHO hopes that the ICD-11 PHC, when it is completed and released, will have greater utility than the ICD-10 PHC was considered to have. But I stress again, that the ICD-11 PHC will be a
non mandatory guideline and its content does not override the ICD-10 and ICD-11 code sets.
It is not possible to predict the extent of the take-up of the ICD-11 PHC or which member states might make use of it in primary care settings.
WONCA's
ICPC-2 (
International Classification of Primary Care, Second edition) has established use as a primary care terminology in a number of member states and it includes
terminology for both mental disorders and general medical conditions - as opposed to the ICD-10 PHC (1996), which contains just 25 "common mental disorders."
As mentioned in my previous post, the SNOMED CT terminology system includes the Concept terms:
Unexplained symptoms continue (finding) and
Medically unexplained symptom (finding). The SNOMED CT UK Edition additionally includes the Concept term:
Medically unexplained symptoms (finding), which is exclusive to the UK Edition and is assigned a different Concept code. No definitions accompany these SNOMED CT terms.
SNOMED CT SCTID codes map to ICD-10 codes and these three codes are mapped to ICD-10 R codes (the
Symptoms, signs chapter).
SNOMED CT includes dozens of Concept terms under (finding) which correspond to the ICD-10
Symptoms, signs R codes.
So there are many codes in both systems that can be used to record symptoms for which no diagnosis classifiable elsewhere is recorded.
This is the text from the WHO's ICD-10 Chapter XVIII Symptoms, signs:
https://icd.who.int/browse10/2016/en#/XVIII
Chapter XVIII
Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified
(R00-R99)
This chapter includes symptoms, signs, abnormal results of clinical or other investigative procedures, and ill-defined conditions regarding which no diagnosis classifiable elsewhere is recorded.
Signs and symptoms that point rather definitely to a given diagnosis have been assigned to a category in other chapters of the classification. In general, categories in this chapter include the less well-defined conditions and symptoms that, without the necessary study of the case to establish a final diagnosis, point perhaps equally to two or more diseases or to two or more systems of the body. Practically all categories in the chapter could be designated 'not otherwise specified', 'unknown etiology' or 'transient'. The Alphabetical Index should be consulted to determine which symptoms and signs are to be allocated here and which to other chapters. The residual subcategories, numbered .8, are generally provided for other relevant symptoms that cannot be allocated elsewhere in the classification.
The conditions and signs or symptoms included in categories R00-R99 consist of:
- cases for which no more specific diagnosis can be made even after all the facts bearing on the case have been investigated;
- signs or symptoms existing at the time of initial encounter that proved to be transient and whose causes could not be determined;
- provisional diagnoses in a patient who failed to return for further investigation or care;
- cases referred elsewhere for investigation or treatment before the diagnosis was made;
- cases in which a more precise diagnosis was not available for any other reason;
- certain symptoms, for which supplementary information is provided, that represent important problems in medical care in their own right.
Excl.:
abnormal findings on antenatal screening of mother (
O28.-)
certain conditions originating in the perinatal period (
P00-P96)
R00-R09 Symptoms and signs involving the circulatory and respiratory systems
R10-R19 Symptoms and signs involving the digestive system and abdome
R20-R23 Symptoms and signs involving the skin and subcutaneous tissue
R25-R29 Symptoms and signs involving the nervous and musculoskeletal systems
R30-R39 Symptoms and signs involving the urinary system
R40-R46 Symptoms and signs involving cognition, perception, emotional state and behaviour
R47-R49 Symptoms and signs involving speech and voice
R50-R69 General symptoms and signs
R70-R79 Abnormal findings on examination of blood, without diagnosis
R80-R82 Abnormal findings on examination of urine, without diagnosis
R83-R89 Abnormal findings on examination of other body fluids, substances and tissues, without diagnosis
R90-R94 Abnormal findings on diagnostic imaging and in function studies, without diagnosis
R95-R99 Ill-defined and unknown causes of mortality
If you are in the US, there is similar text at the beginning of ICD-10-CM
Chapter 18: Symptoms, signs etc.
--------------------
(My highlighting below)
http://www.londonhp.nhs.uk/wp-content/uploads/2011/03/MUS-whole-systems-approach.pdf
Medically Unexplained Symptoms (MUS)
A whole systems approach
July 2009 – December 2010
Page 20
"It may be possible within the new polyclinic model that the routine of psychologists working
with consultants would develop. Equally, they could work in hospitals in more structured ways
such as a ‘pelvic pain’ clinic.
"We would suggest that one consultant in each department should lead on this area of the
work, helping other consultants to think about difficult presentations, ensuring patients can
access the psychologist appropriately and reviewing the care of patients where no biological
explanation can be found. At present, patients are referred back to primary care or on to
another secondary care department, thus allowing the clinician to maintain the idea that
medically unexplained symptoms are not part of their work.
"It will be necessary for acute clinicians working in these clinics to code patients that they feel
may have MUS. There are often no codes available to do this in these specialities. We would
advise therefore that the ICD codes F44, F45 and F48 are used as ‘catch-all’ codes. These
would include any situation where the clinicians felt there was an element of MUS affecting the
patient and their management. This is necessary in order for outcomes to be quantifiable.
These codes are to be used to monitor outcomes; clinicians can use the codes where
appropriate, in conjunction with other codes."
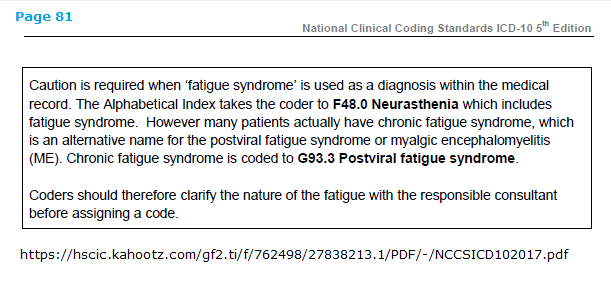
(Note that under
F48.0 Neurasthenia (and its inclusion:
Fatigue syndrome) there is an exclusion (
Excl.) for G93.3.)
Also note:
But there are no exclusions for G93.3 under the ICD-10 F45.x codes.
So an additional F45.x diagnosis can be added to an existing or new diagnosis of G93.3, or to any other disease or condition.
"F45 Somatoform disorders
"The main feature is repeated presentation of physical symptoms together with persistent requests for medical investigations, in spite of repeated negative findings and reassurances by doctors that the symptoms have no physical basis. If any physical disorders are present, they do not explain the nature and extent of the symptoms or the distress and preoccupation of the patient."
I have heard from several patients over the years (and prior to the development and roll-out of IAPT, MUS and PPS services) who have told me that in their medical records they had been assigned an F45.x code in addition to the G93.3 code.
For ICD-11, again, no specific term for "Medically unexplained symptoms."
Bodily distress disorder replaces most of the ICD-10
Somatoform disorder categories and also subsumes and replaces F48.0
Neurasthenia.
Like DSM-5's SSD, there is no longer the requirement for the chronic, distressing symptoms to be "medically unexplained." A patient may be diagnosed with BDD, or an
additional diagnosis of BDD can be added in the presence of a general medical condition or disease:
"...If another health condition is causing or contributing to the symptoms, the degree of attention is clearly excessive in relation to its nature and progression."
The criteria set for DSM-5's SSD and the more flexible disorder description texts for ICD-11's conceptualization of BDD are considerably looser and more easily met than the
Somatoform disorders they replace.
This makes BDD very problematic for ME and CFS patients and I continue to push for exclusions for the three G93.3 legacy terms. Proposals for exclusions under BDD have been recently processed and rejected [1].
So in brief response to your question: in the UK NHS there is no mandatory ICD classification system that includes a coded for (or defined) term "Medically unexplained symptoms", there is no consensus definition, and there are other ICD-10 codes (in the R code chapter) that can be used for the recording of symptoms where no firm diagnosis can be recorded, which may be transitory symptoms, or prodromal symptoms.
1
Status of ICD-11 processed proposals v1:
https://dxrevisionwatch.com/status-of-icd-11-processed-proposals-v1/