Don't think this was one has been increased much in ME/CFS? IL-10 was in some but not many. TGF-beta has been the most consistent one but even there many inconsistent results.
For comparison to ME/CFS, just made this brief summary of the cytokine literature on social media
1) Been looking at cytokines; small signalling molecules of the immune system.
Conclusion: lots of ME/CFS studies on this but inconsistent results. There doesn't seem to be an inflammatory cytokine response (in the blood).
Most consistently elevated cytokine was TGF-beta.
2) The table attached is from an outdated review from 2015, but it still includes most of the major cytokines studies in ME/CFS as these were done years ago.
https://sciencedirect.com/.../abs/pii/S088915911500238X
Interest in cytokine levels seems to have dwindled due to inconsistent results.
3) One of the major studies that came out afterwards was the Montoya study from 2017, published in PNAS. Almost 200 ME/CFS patients were tested at Stanford. TGF-β was also elevated compared to controls.
Link:
https://www.pnas.org/doi/10.1073/pnas.1710519114
4) But there was a paradox in this study. TGF-β was increased but didn't correlate with ME/CFS severity. Several inflammatory cytokines such as IFN-gamma on the other hand did correlate with ME/CFS severity but levels were similar to controls.
5) Another major study was done by Mady Hornig and colleagues at Columbia, published in 2015. It had a large sample size: 298 patients and 348 controls. Here, patients often had lower levels of circulating cytokines.
https://www.science.org/doi/10.1126/sciadv.1400121
6) But zooming in, the researchers found a pattern: patients with a short illness duration (≤3 years) did have increased cytokine levels than controls while those with long duration had lower levels.
7) In other words, there seems to be a trajectory. Early in the illness ME/CFS patients might show (slightly) elevated cytokine levels but this immune signature disappears over time.
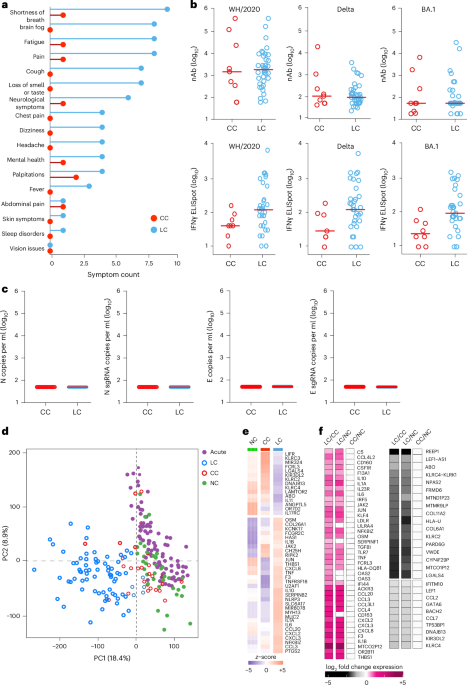
8) This as an exploratory analysis but it would fit with Long Covid studies having more success at finding increased inflammatory markers such as IL-6 and TNF-alpha. They all tested patients relatively early after the immune trigger.
Link:
https://www.nature.com/articles/s41590-025-02353-x
9) A few words about TGF-beta, the cytokine most consistently found to be elevated in ME/CFS.
It is a multifunctional cytokine: it's meaning and function depends on the context. But it often works as an anti-inflammatory signal, a break to the immune response.
10) TGF-beta, for example, promotes the production of extracellular matrix proteins and helps with tissue repair.
In fibrosis, TGF-beta is overactive.
https://sciencedirect.com/.../article/pii/S0092867423008516
11) There are also quite a few ME/CFS studies that did NOT find increase TGF-beta such as the Hornig study above and the ones below:
Wyller et al. 2017:
https://link.springer.com/article/10.1186/s12967-017-1350-1
Roerink et al. 2018:
https://njmonline.nl/article_ft.php?a=2020&d=1326&i=218
12) One of the reasons that these studies have become less popular is also because cytokines are influenced by multiple factors such as sex, age, BMI, time of measurement, etc.
13) Cytokines only have a local effect, usually near an infection or injury. They aren't hormones that are meant to travel and pass on info throughout the body. What we see in the blood is likely spillover of a local increase somewhere, a weak echo of what's going on.
14) This 2019 review by Michael VanElzakker gives a good overview of research methods and limitations in measuring cytokines.
Link:
https://www.frontiersin.org/.../10.../fneur.2018.01033/full
15) Absolute cytokine measurements often differ per testing kit used and time of sampling. So when comparing studies, only the relative effect compared to controls that were sampled in the exact same way, gives useful info.
16) There are also a couple of studies that measured cytokines not in plasma or blood but in the cerebrospinal fluid that surrounds the brain.
Unfortunately these often have much smaller sample sizes, making it even more difficult to get consistent results.