Just as a side note, I found the statistics about people in the Canadian ME/CFS cohort on the MFI-20 a bit interesting - see
@wigglethemouse's
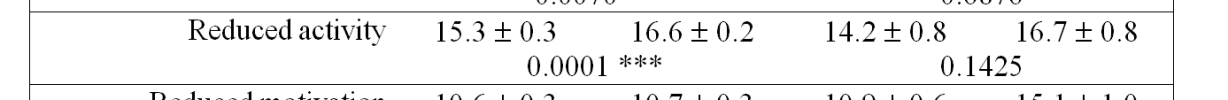
post of the table upthread. A total score of MFI-20 of over 60 is regarded as indicating unusual levels of fatigue. There are 5 sub-sets of fatigue, each with a maximum score of 20 and a minimum of 4, and so a score of up to a bit over 10 on one of the subsets is still well within normal bounds.
General fatigue and physical fatigue are up around 16 and 17 out of 20 for the cohort, presumably way out on the end of a population distribution. Reduced activity is mostly around 16 out of 20. Mental fatigue is about 14.
But the scores for reduced motivation are way less than other measures of fatigue, for both men and women.
The female mean score (regardless of SMPDL3B levels) for 'reduced motivation' is 10.65. The male mean score is 12.23, with there looking to be quite a strong positive relationship with overall severity and a lot more individual variation.
So, self-reported reduced motivation does not seem to be a major component of self-reported fatigue in this ME/CFS cohort.
The exception is the group of 13 men who have a high mean overall fatigue level. Their mean score for reduced motivation is 15.1. Now, of course, this is a very small number of people and I know I'm somewhat torturing the data until it tells me what I want to hear. But, it looks as though there is a significant proportion of the male group with quite high reduced motivation scores. My personal experience contributes to me thinking that men may be more likely to explain their incapacity away by saying that they didn't really want to do the activity, that they could not be bothered. A sort of 'show no weakness' attitude, even to the point of preferring to be seen as lazy than explaining to people that they are ill. Not all men, of course. It's possible that that higher reduced motivation score is related to depression too.
A person who thinks that they are probably just unmotivated is less likely to go to see a doctor and even less likely to actually get an ME/CFS diagnosis. A man who reports feeling depressed as well may be even less likely to get an ME/CFS diagnosis, which is often seen as a female disease.
I think it's a phenomenon worth watching out for, because it may help to explain some of the sex ratio skew to female predominance in diagnosed ME/CFS.