I'm just a patient, sick since 1990, who is sharing some thoughts. I hope this makes some kind of sense.
Right now, those who work on your behalf to support the disease model use CFS as the term for the psych alternative. That approach works in your favor.
I think that first statement is wrong. I don't think that most researchers who work on this illness [ME/CFS/SEID/PVFS?/etc] use CFS as "the term for the psych alternative."
But even if I agreed that we could somehow improve life for ME patients by just changing the term CFS to mean "
a psychiatric condition that sometimes develops in reaction to acute viral infection" I still would not throw CFS patients under the bus just to help myself. That would be cruel!
That said, I'm probably one of the patients who would get thrown under the bus.
I live in the USA. When I filed for disability benefits with the SSA [Social Security Association], back in the year 2000, my illness was coded as
Chronic Fatigue Syndrome. (I've linked to an SSA webpage which now includes the term ME - but that term was
not used on the SSA website 20 years ago when I applied for disability benefits).
For what it's worth, I meet several other
diagnostic criteria for ME, not just the Fukuda CFS criteria. I don't think that would help me much.
Folks in the USA who have a CFS diagnosis, and who are also on disability benefits, have a hard enough time as it is. We have to provide loads of evidence just to qualify for disability benefits. We have to be seen by one of the SSA doctors. These SSA doctors often manage to get valid claims denied. Even if we make it through the gauntlet of forms/tests/etc, every time our disability claim comes up for review (every 3-5 years for an average CFS patient) we have to provide more evidence, maybe go back for more doctor appointments, more medical evidence, or get another letter from the doctor, and so on.
The SSA is underfunded. There is a backlog of cases to be approved and reviewed. To top it all off, the president of the USA keeps talking about
tax cuts that would bankrupt the SSA funds.
The idea that doctors and insurance companies would suddenly change terminology and start using CFS as "the term for the psych alternative" is absolutely terrifying!
Folks in the USA with a CFS diagnosis in their medical files, as well as in their SSA files, would have to fight
both their own doctors and the SSA bureaucracy to change their diagnostic name to ME. And then fight with their insurance companies (we don't have national health care) on top of that.
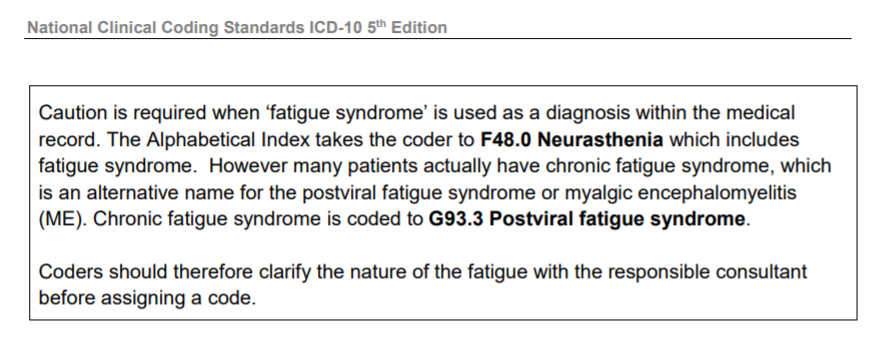
Disease coding is important, yes, but ignore coding for a minute. I'm just talking about the name CFS being associated with a psychiatric diagnosis for every single patient who has that label in their files. I can't even IMAGINE how much work it would take to get that label out of their files and changed to ME! I think many patients would simply give up.
But even if this idea hurt no one, even if someone could snap their fingers and magically make all those bureaucratic changes happen -- everyone's CFS diagnosis is changed to ME (or ME/CFS), no one loses their disability benefits, everyone continues to get insurance coverage for their doctor appointments and prescriptions -- I would STILL not agree with this idea.
I could not in good conscience support the idea that the term CFS refers to a psychiatric diagnosis.
Patients with a Chronic Fatigue Syndrome diagnosis, or a Chronic Fatigue (CF) diagnosis, or even an ME diagnosis, might not have ME (or CFS or SEID). People get diagnosed incorrectly all the time. There are a lot of unknowns.
But I do not think there is a group of psychiatric patients with a diagnosis of CFS that is "
essentially deconditioning that arises from inactivity when patients embrace faulty illness beliefs." I have not seen any proof for this.
[final edit to fix a couple of typos]