Myopathy as a cause of fatigue in long-term post-COVID-19 symptoms: Evidence of skeletal muscle histopathology
Eva K Hejbøl, Thomas Harbo, Jane Agergaard, Line B Madsen, Thomas H Pedersen, Lars J Østergaard, Henning Andersen, Henrik D Schrøder, Hatice Tankisi
Background: Among post-COVID-19 symptoms, fatigue is reported as one of the most common, even after mild acute infection, and as the cause of fatigue, myopathy diagnosed by electromyography has been proposed in previous reports. This study aimed to explore the histopathological changes in patients with post-COVID-19 fatigue.
Methods: Sixteen patients (mean age:46 years) with post-COVID-19 complaints of fatigue, myalgia or weakness persisting for up to 14 months were included. In all patients, quantitative electromyography and muscle biopsies analysed with light and electron microscopy were taken.
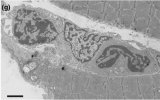
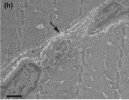
Results: Muscle weakness was present in 50%, myopathic electromyography in 75% while in all patients, there were histological changes. Muscle fiber atrophy was found in 38%, and 56% showed indications of fiber regeneration. Mitochondrial changes, comprising loss of COX activity, subsarcollemmal accumulation and/or abnormal cristae, were present in 62%. Inflammation was found in 62%, seen as T-lymphocytes and/or muscle fiber HLA-ABC expression. In 75%, capillaries were affected involving basal lamina and cells. In two patients, uncommon amounts of basal lamina were found, not only surrounding muscle fibers but also around nerves and capillaries.
Conclusions: The wide variety of histological changes in this study suggest that skeletal muscles may be a major target of SARS-CoV-2 causing muscular post-COVID-19 symptoms. The mitochondrial changes, inflammation and capillary injury in muscle biopsies can cause fatigue in part due to reduced energy supply. Since most patients had mild-moderate acute affection, the new variants that might cause less severe acute disease could still have the ability to cause long-term myopathy.
Link (paywalled)
Eva K Hejbøl, Thomas Harbo, Jane Agergaard, Line B Madsen, Thomas H Pedersen, Lars J Østergaard, Henning Andersen, Henrik D Schrøder, Hatice Tankisi
Background: Among post-COVID-19 symptoms, fatigue is reported as one of the most common, even after mild acute infection, and as the cause of fatigue, myopathy diagnosed by electromyography has been proposed in previous reports. This study aimed to explore the histopathological changes in patients with post-COVID-19 fatigue.
Methods: Sixteen patients (mean age:46 years) with post-COVID-19 complaints of fatigue, myalgia or weakness persisting for up to 14 months were included. In all patients, quantitative electromyography and muscle biopsies analysed with light and electron microscopy were taken.
Results: Muscle weakness was present in 50%, myopathic electromyography in 75% while in all patients, there were histological changes. Muscle fiber atrophy was found in 38%, and 56% showed indications of fiber regeneration. Mitochondrial changes, comprising loss of COX activity, subsarcollemmal accumulation and/or abnormal cristae, were present in 62%. Inflammation was found in 62%, seen as T-lymphocytes and/or muscle fiber HLA-ABC expression. In 75%, capillaries were affected involving basal lamina and cells. In two patients, uncommon amounts of basal lamina were found, not only surrounding muscle fibers but also around nerves and capillaries.
Conclusions: The wide variety of histological changes in this study suggest that skeletal muscles may be a major target of SARS-CoV-2 causing muscular post-COVID-19 symptoms. The mitochondrial changes, inflammation and capillary injury in muscle biopsies can cause fatigue in part due to reduced energy supply. Since most patients had mild-moderate acute affection, the new variants that might cause less severe acute disease could still have the ability to cause long-term myopathy.
Link (paywalled)