Ryan31337
Senior Member (Voting Rights)
Full title: Neutralization of Autoantibodies Targeting G-Protein Coupled Receptors Improves Capillary Impairment and Fatigue Symptoms after COVID-19 Infection
Abstract
Clinical features of Corona Virus Disease 2019 (COVID-19) are caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Acute infection management is a substantial health care issue, and the development of a Long-Covid syndrome (LCS) is extremely challenging for patients and physicians. It is associated with a variety of characteristics as e.g. impaired capillary microcirculation, chronic fatigue syndrome (CFS) and functional autoantibodies targeting G-protein coupled receptors (GPCR-AAb).
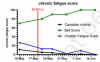
Here, we present a case report of a successful healing of LCS with BC 007 (Berlin Cures, Berlin, Germany), a DNA aptamer drug with high affinity to GPCR-AAbs that neutralizes these AAbs. A patient with a documented history of glaucoma, recovered from mild COVID-19, but still suffered from chronic fatigue syndrome, loss of taste and impaired capillary microcirculation in the macula and peripapillary region. He was positively tested for various targeting GPCR-AAbs. Within 48 h after a single BC 007 treatment, GPCR-AAbs were functionally inactivated and remained inactive during the observation period of 4 weeks.
This observation was accompanied by a constant improvement of the patient’s fatigue symptoms, and taste as well as retinal capillary microcirculation. This phenotype is, to the best of our knowledge, the first report worldwide of a direct cure of symptoms of LCS. Therefore, we propose that removal of GPCR-AAb ameliorates characteristics of the Long-Covid-Syndrome such as capillary impairment, loss of taste and CFS.
Open access, https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3879488
Abstract
Clinical features of Corona Virus Disease 2019 (COVID-19) are caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Acute infection management is a substantial health care issue, and the development of a Long-Covid syndrome (LCS) is extremely challenging for patients and physicians. It is associated with a variety of characteristics as e.g. impaired capillary microcirculation, chronic fatigue syndrome (CFS) and functional autoantibodies targeting G-protein coupled receptors (GPCR-AAb).
Here, we present a case report of a successful healing of LCS with BC 007 (Berlin Cures, Berlin, Germany), a DNA aptamer drug with high affinity to GPCR-AAbs that neutralizes these AAbs. A patient with a documented history of glaucoma, recovered from mild COVID-19, but still suffered from chronic fatigue syndrome, loss of taste and impaired capillary microcirculation in the macula and peripapillary region. He was positively tested for various targeting GPCR-AAbs. Within 48 h after a single BC 007 treatment, GPCR-AAbs were functionally inactivated and remained inactive during the observation period of 4 weeks.
This observation was accompanied by a constant improvement of the patient’s fatigue symptoms, and taste as well as retinal capillary microcirculation. This phenotype is, to the best of our knowledge, the first report worldwide of a direct cure of symptoms of LCS. Therefore, we propose that removal of GPCR-AAb ameliorates characteristics of the Long-Covid-Syndrome such as capillary impairment, loss of taste and CFS.
Open access, https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3879488
Last edited by a moderator: