Sly Saint
Senior Member (Voting Rights)
The IAPT Double Myth of Economic and Clinical Utility
http://www.cbtwatch.com/the-iapt-double-myth-of-economic-and-clinical-utility/
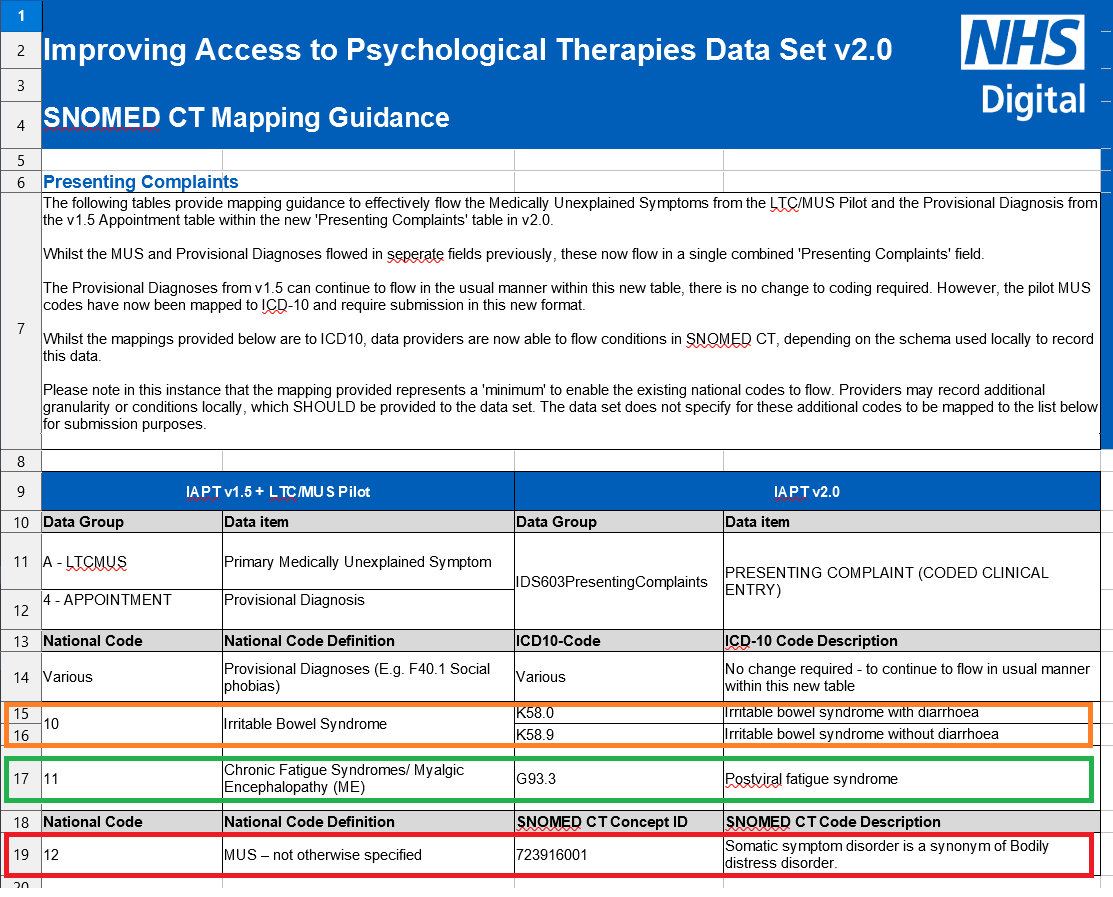
There is not just a gap between the psychological treatments delivered in randomised controlled trials and what comes to pass in routine psychological services, such as the Improving Access to Psychological Therapies Programme (IAPT) service, but a chasm. Efforts to have a meaningful debate on the issue have been met with a deafening silence. In the silence, the scope of psychological treatments has gradually been expanded, beyond the initial focus of depression and the anxiety disorders to include patients with long term physical conditions – a psychological imperialism. The power-holders definition of the outcome of routine psychological treatment reigns.
http://www.cbtwatch.com/the-iapt-double-myth-of-economic-and-clinical-utility/